Kronik obstrüktif akciğer hastalığı: Revizyonlar arasındaki fark
| [kontrol edilmiş revizyon] | [kontrol edilmiş revizyon] |
→Sağaltım (tedavi): Yazım hatası düzeltildi Etiketler: referans etiketleri kaldırıldı Mobil değişiklik mobil uygulama değişikliği |
kDeğişiklik özeti yok |
||
| 1. satır: | 1. satır: | ||
{{çalışma}} |
|||
{{tıpUyarı}} |
{{tıpUyarı}} |
||
<br /> |
|||
{{Hastalık bilgi kutusu |
{{Hastalık bilgi kutusu |
||
| Hastalık adı |
| Hastalık adı = Kronik obstrüktif akciğer hastalığı |
||
| Resim |
| Resim = [[Dosya:Centrilobular emphysema 865 lores.jpg|thumb]] |
||
| Resim açıklama = Sigara içme durumunda tipik olarak görülen santrilobüler tip amfizemde, akciğerin [[gros patoloji]]si. Bu kesilmiş [[fiksasyon (histoloji)|fiksaj]]ın yakından görünümünde, boşluklara dolmuş yoğun noktasal [[siyah karbon]] tortuları görülmektedir. |
|||
| Resim açıklama = Koah'ta bir akciğerin patolojik görüntüsü |
|||
| Hastalık Veri Tabanı = 2672 |
| Hastalık Veri Tabanı = 2672 |
||
| |
| ICD10 kodu = {{ICD10|J|40||j|40}}–{{ICD10|J|44||j|40}}, {{ICD10|J|47||j|40}} |
||
| |
| ICD9 kodu = {{ICD9|490}}–{{ICD9|492}}, {{ICD9|494}}–{{ICD9|496}} |
||
| |
| OMIM = 606963 |
||
| MedlinePlus |
| MedlinePlus = 000091 |
||
| eMedicineKonu |
| eMedicineKonu = med |
||
| eMedicineBaşlık |
| eMedicineBaşlık = 373 |
||
| eMedicine_çoklu |
| eMedicine_çoklu = {{eMedicine2|emerg|99}} |
||
| |
| Meshİsmi = COPD |
||
| MeshNumarası = C08.381.495.389 |
|||
| MeshID = D009447 |
|||
| Meshİsmi = |
|||
| MeshNumarası = C08.381.495.389 |
|||
}} |
}} |
||
<!--Tanım ve semptomlar --> |
|||
[[Dosya:Copd_versus_healthy_lung.jpg|right|thumb|KOAH'ın canlandırma çizimi]] |
|||
'''Kronik obstrüktif akciğer hastalığı''' ('''KOAH'''), zayıf hava akışının görüldüğü [[obstrüktif akciğer hastalığı|obstrüktif]] bir akciğer hastalığıdır.<!-- <ref name=GOLD2013Chp1/> --> Tipik olarak zamanla daha kötüleşir.<!-- <ref name=GOLD2013Chp1/> --> Ana belirtileri [[nefes darlığı]], [[öksürme]] ve [[balgam]] üretimidir.<ref name=GOLD2013Chp1/> '''Kronik bronşit''' sahibi insanların çoğu aynı zamanda KOAH hastasıdır.<ref name=Harr2012/> |
|||
<!--Neden ve teşhis --> |
|||
'''Kronik Obstrüktif Akciğer Hastalığı (KOAH)''', ('''süreğen tıkanan akciğer hastalığı''') bir akciğer hastalığıdır. |
|||
[[Tütün içiciliği]] hastalığın en temel nedeni olup [[hava kirliliği]] ve [[genetik]] gibi daha az etkili nedenleri de vardır.<ref name=Lancet2012>{{cite journal |author=Decramer M, Janssens W, Miravitlles M |title=Chronic obstructive pulmonary disease |journal=Lancet |volume=379 |issue=9823 |pages=1341–51 |date=Nisan 2012 |pmid=22314182 |doi=10.1016/S0140-6736(11)60968-9}}</ref> Gelişmekte olan ülkelerde, hava kirliliğinin en etkili nedenlerinden biri doğru havalandırılmamış yemek pişirme ve ısıtma ateşi dumanıdır. Bu tahriş edici şeylere uzun süreli maruz kalmalar, akciğerlerde [[iltihap]]lanmaya neden olarak küçük hava yollarının daralmasına ve '''amfizem''' adı verilen doku parçalanmasına yol açar.<ref name=GOLD2007>{{cite journal | author = Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J | title = Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary | journal = Am. J. Respir. Crit. Care Med. | volume = 176 | issue = 6 | pages = 532–55 |date=Eylül 2007 | pmid = 17507545 | doi = 10.1164/rccm.200703-456SO | url = http://ajrccm.atsjournals.org/content/176/6/532.long }}</ref> Teşhis, zayıf hava akışını kontrol eden [[akciğer fonksiyon testleri]] ile anlaşılır.<ref name=Nathell>{{cite journal | author = Nathell L, Nathell M, Malmberg P, Larsson K | title = COPD diagnosis related to different guidelines and spirometry techniques | journal = Respir. Res. | volume = 8 | issue = 1| pages = 89 | year = 2007 | pmid = 18053200 | pmc = 2217523 | doi = 10.1186/1465-9921-8-89 }}</ref> [[Astım]]dan farklı olarak, KOAH hastalarında hava akışı herhangi bir ilaç yardımıyla belirgin bir şekilde düzelemez. |
|||
<!-- Önlem ve yönetim --> |
|||
KOAH, bilinen nedenlere maruz kalınımı düşürerek önlenebilir. Bunlar arasında sigara içme oranlarını azaltmak ve iç/dış hava kalitesini yükseltmek gösterilebilir. KOAH tedavileri [[sigarayı bırakma]], [[aşı]]lar, [[akciğer rehabilitasyonu|rehabilitasyon]], sıkça içe çekilen [[bronkodilatör]]ler ve [[kortikosteroit|steroit]]ler içerir. Bazı insanlar, [[oksijen terapisi|uzun süreli oksijen terapisi]] veya [[akciğer nakli]]yle belirgin iyileşmeler gösterebilir.<ref name=GOLD2007/> [[Kronik obstrüktif akciğer hastalığında akut şiddetlenme|Akut kötüleşme]] periyotları gösteren hastalarda, artan oranlarda ilaç ve hastane altında gözetim gerekebilir. |
|||
<!--Epidemiology --> |
|||
Halk dilinde "kronik bronşit", "müzmin bronşit" gibi adlarla bilinen KOAH, akciğerlerdeki hava yollarının daralmasına bağlı olarak soluk alıp verme sırasında hava akımının kısıtlanması ile nitelenen süreğen (kronik) bir hastalıktır. |
|||
Dünya çapında KOAH, 329 milyon insanı (dünya nüfusunun %5'i) etkilemektedir. 2012'de 3 milyon insanın ölümüne sebebiyet vererek, dünyadaki en ölümcül üçüncü hastalık olarak tanımlandı.<ref name="WHOTTCD">{{cite web |title=The 10 leading causes of death in the world, 2000 and 2011 |date=July 2013 |publisher=World Health Organization |url=http://who.int/mediacentre/factsheets/fs310/en/ |accessdate=29 Kasım 2013}}</ref> Ölümlerin, yükselen sigara kullanımı ve bazı ülkelerdeki yaşlanan nüfus nedeniyle daha da artacağı öngörülmektedir.<ref>{{cite journal |author=Mathers CD, Loncar D |title=Projections of Global Mortality and Burden of Disease from 2002 to 2030 |journal=PLoS Med. |volume=3 |issue=11 |pages=e442 |date=November 2006 |pmid=17132052 |pmc=1664601 |doi=10.1371/journal.pmed.0030442 |url=http://dx.plos.org/10.1371/journal.pmed.0030442}}</ref> 2010'da hastalığın 2.1 trilyon dolarlık bir ekonomik zarara yol açtığı tahmin edildi.<ref name=Cost2013>{{cite book|last=Lomborg|first=Bjørn|title=Global problems, local solutions : costs and benefits|year=2013|publisher=Cambridge University Pres|isbn=978-1-107-03959-9|page=143|url=http://books.google.ca/books?id=cRZaAQAAQBAJ&pg=PA143}}</ref> |
|||
{{TOC limit|3}} |
|||
[[Amfizem]] ve kronik [[bronşit]]i kapsayan bir hastalık öbeğine giren Kronik Obstrüktif Akciğer Hastalığı'nın en önemli özelliği, akciğerlere giren ve çıkan havayı, soluk darlığına neden olacak kadar kısıtlayabilmesidir. KOAH nedeniyle dünyada her yıl yaklaşık 2.500.000 kişi yaşamını yitirmektedir. Dünya genelinde ölüm nedenleri arasında altıncı sırada yer alan Kronik Obstrüktif [[Akciğer]] Hastalığı'nın artış oranı % 163 gibi yüksek bir sayıdır. |
|||
== Belirtiler ve semptomlar == |
|||
Kalıtsal özellikleri de görülen KOAH'ın yarattığı hava akımının engellenmesinin nedeni; akciğerlerde gelişen yangının (enflasmasyonun) yol açtığı asaldoku (parenkim) harabiyeti (amfizem) ve/ya da küçük hava yollarındaki daralma ve bronş çevresindeki liflenmedir (peribronşiyal fibrozis, küçük hava yolu hastalığı). |
|||
{{dinle |
|||
| dosyaismi = Wheeze2O.ogg |
|||
| başlık = Hırıltı |
|||
| açıklama = Stetoskop ile dinlenen hırıltı sesleri. |
|||
| format = [[Ogg]] |
|||
}} |
|||
KOAH'ın en belirgin belirtisi balgam üretimi, [[nefes darlığı]] ve sık öksürmelerdir.<ref name=GOLD2013Chp2>{{cite book |last=Vestbo |first=Jørgen |title=Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease |year=2013 |publisher=Global Initiative for Chronic Obstructive Lung Disease |pages=9–17 |chapter=Diagnosis and Assessment |chapterurl=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf#26}}</ref> Bu belirtiler, uzun sürelere yayılmış bir şekilde görülür<ref name=Harr2012>{{cite book |first1=John J. |last1=Reilly |first2=Edwin K. |last2=Silverman |first3=Steven D. |last3=Shapiro |chapter=Chronic Obstructive Pulmonary Disease |pages=2151–9 |editor1-first=Dan |editor1-last=Longo |editor2-first=Anthony |editor2-last=Fauci |editor3-first=Dennis |editor3-last=Kasper |editor4-first=Stephen |editor4-last=Hauser |editor5-first=J. |editor5-last=Jameson |editor6-first=Joseph |editor6-last=Loscalzo |year=2011 |title=Harrison's Principles of Internal Medicine |edition=18th |publisher=McGraw Hill |isbn=978-0-07-174889-6}}</ref> ve tipik olarak zamanla kötüleşir.<ref name=GOLD2007/> KOAH'ın farklı tiplerinin olup olmadığı kesinleştirilmiş değildir.<ref name=Lancet2012/> Önceden amfizem ve kronik bronşit olarak ayrılan hastalıkta, amfizem aslında bir hastalıktan ziyade akciğerdeki değişimleri belirtmek adına kullanılır. Kronik bronşit ise, KOAH hastalığına eşlik edip etmeyeceği kesin olmayan, sadece bazı belirtileri açıklayan bir terimdir.<ref name=GOLD2013Chp1>{{cite book |last=Vestbo |first=Jørgen |title=Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease |year=2013 |publisher=Global Initiative for Chronic Obstructive Lung Disease |pages=1–7|chapter=Definition and Overview |chapterurl=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf#18}}</ref> |
|||
=== Öksürme === |
|||
Kronik öksürmeler gözlenebilen ilk belirtilerdir.<!-- <ref name=GOLD2013Chp2/> --> İki yıldan uzun bir sürede, yılda üç aydan fazla süren ve balgam üretiminin eşlik ettiği durum, fazladan herhangi bir açıklama yapılmadığı sürece kronik bronşit tanımına dahil olur.<!-- <ref name=GOLD2013Chp2/> --> Bu durum, KOAH tamamen başlamadan önce de görülebilir.<!-- <ref name=GOLD2013Chp2/> --> Üretilen balgam miktarı, saatler veya günler arasında farklılık gösterebilir.<!-- <ref name=GOLD2013Chp2/> --> Bazı durumlarda, öksürük görülmeyebilir ve sıklıkla gözlenmeyen bir biçimde rastlanılabilir.<!-- <ref name=GOLD2013Chp2/> --> Bazı insanlar bu belirtileri sigaraya atfederler.<!-- <ref name=GOLD2013Chp2/> --> Balgam, toplumsal ve kültürel koşullara göre yutulup tükürülebilir.<!-- <ref name=GOLD2013Chp2/> --> Kuvvetli öksürmeler [[kaburga kırılması]] veya [[Senkop (tıp)|kısa süreli bilinç kaybı]]na sebebiyet verebilir.<!-- <ref name=GOLD2013Chp2/> --> KOAH tanısı konulan insanların genelde uzun süren "[[nezle]]" geçmişleri vardır.<ref name=GOLD2013Chp2/> |
|||
=== Nefes kesilmesi === |
|||
Nefes darlığı hastaların en çok şikayet ettiği belirtidir.<ref name=NICE2010P60>{{NICE|101|Chronic Obstructive Pulmonary Disease|June 2010|60-70}}</ref> Bu durum sıklıkla şöyle tanımlanır: "zorlukla nefes alıyorum", "nefesim kesiliyor" veya "yeterince hava alamıyorum".<ref name=Mahler2006>{{cite journal |author=Mahler DA|title=Mechanisms and measurement of dyspnea in chronic obstructive pulmonary disease |journal=Proceedings of the American Thoracic Society|volume=3 |issue=3 |pages=234–8 |year=2006 |pmid=16636091 |doi=10.1513/pats.200509-103SF}}</ref> Ancak farklı terimler farklı kültürlerde kullanılabilir.<ref name=GOLD2013Chp2/> Tipik olarak nefes darlığı, uzun süreli güç harcama durumlarında daha kötü bir hal alır ve zamanla kötüleşir.<ref name=GOLD2013Chp2/> İleri vakalarda dinlenme sırasında da gözlenebilir ve sürekli gözlenebilir.<ref>{{cite web |title=What Are the Signs and Symptoms of COPD? |date=31 Temmuz 2013 |publisher=[[National Heart, Lung, and Blood Institute]] |url=http://www.nhlbi.nih.gov/health/health-topics/topics/copd/signs.html |accessdate=29 Kasım 2013}}</ref><ref name=MedlinePlus>{{MedlinePlusEncyclopedia|000091|Chronic obstructive pulmonary disease}}</ref> Bu durum, KOAH hastalarının endişe duyduğu ve hayat kalitesini düşüren en başlıca belirtidir.<ref name=GOLD2013Chp2/> Daha ileri düzey KOAH hastaları [[büzük dudak nefesi|büzülmüş dudaklarından nefes alır]] ve bu bazı durumlarda nefes darlığını iyileştirebilir.<ref>{{cite book|last=Morrison|first=[edited by] Nathan E. Goldstein, R. Sean|title=Evidence-based practice of palliative medicine|publisher=Elsevier/Saunders|location=Philadelphia|isbn=978-1-4377-3796-7|page=124|url=http://books.google.ca/books?id=j0rCsKtCnq8C&pg=PA124|year=2013}}</ref><ref name=Holland2012>{{cite journal | author = Holland AE, Hill CJ, Jones AY, McDonald CF | title = Breathing exercises for chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | volume = 10 | pages = CD008250 | year = 2012 | pmid = 23076942 | doi=10.1002/14651858.CD008250.pub2 | editor1-last = Holland | editor1-first = Anne E }}</ref> |
|||
=== Diğer özellikler === |
|||
KOAH hastalarında nefes vermek nefes almaktan uzun sürebilir<ref name=EB2008/> Göğüs sıkışması görülebilir<ref name=GOLD2013Chp2/> ancak çok yaygın değildir ve başka bir durumdan dolayı kaynaklanabilir.<ref name=NICE2010P60/> Nefes yolları engellenmiş hastalar [[hırıltı|hırıldayabilir]] veya nefes alırken [[stetoskop|stetoskoba]] daha az ses verebilir.<ref name=EB2008/> [[Fıçı göğüs]] de KOAH hastalığının karakteristik belirtisidir ancak görece daha az rastlanır.<ref name=EB2008/> [[Tripod pozisyonu]] hastalık kötüleştikçe gözlenebilir.<ref name=Harr2012/> |
|||
İleri düzey KOAH, [[akciğer hipertansiyonu|akciğer arterlerinde yüksek basınca]] neden olabilir ve bu nedenle [[kalp krizi|kalbin sağ karıncığı]]na baskı uygulayabilir.<ref name=GOLD2007/><ref name=Weit2009>{{cite journal | author = Weitzenblum E, Chaouat A | title = Cor pulmonale | journal = Chron Respir Dis | volume = 6 | issue = 3 | pages = 177–85 | year = 2009 | pmid = 19643833 | doi = 10.1177/1479972309104664 }}</ref><ref>{{cite book |title=Professional guide to diseases |year=2009 |publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins |location=Philadelphia |isbn=978-0-7817-7899-2 |pages=120–2 |chapter=Cor pulmonale |chapterurl=http://books.google.ca/books?id=1h6vu60L6FcC&pg=PA120 |edition=9th}}</ref> [[Cor pulmonale]] olarak adlandırılan bu durum, [[çevresel ödem|bacak şişmesi]]ne <ref name=GOLD2013Chp2/> ve [[boyun damarı distansiyonu|şişen boyun damarı]]na neden olabilir.<ref name=GOLD2007/> KOAH, diğer bütün akciğer hastalıklarından daha büyük bir ''cor pulmonale'' tetikleyicisidir.<ref name=Weit2009/> Ancak, cor pulmonale, oksijen tedavisinin kullanımından beri daha az yaygındır.<ref name=Harr2012/> |
|||
KOAH, daha çok paylaşılan risk faktörleri nedeniyle, diğer bazı durumlarla beraber gerçekleşir.<ref name=Lancet2012/> Bunlar arasında [[koroner arter hastalığı]], [[hipertansiyon|yüksek kan basıncı]], [[diyabet]], kas yıkımı, [[osteoporoz]], [[akciğer kanseri]], [[anksiyete bozukluğu]] ve [[majör depresif bozukluk|depresyon]] yer alır.<ref name=Lancet2012/> Ciddi hastalıkları olan insanlarda [[hâlsizlik]] yaygın görülür.<ref name=GOLD2013Chp2/> [[Çomak parmak]], KOAH'ya özgü değildir ve altta yatan bir [[akciğer kanseri]] için araştırmaları tetiklemelidir.<ref>{{cite book|last=Mandell|first=editors, James K. Stoller, Franklin A. Michota, Jr., Brian F.|title=The Cleveland Clinic Foundation intensive review of internal medicine|year=2009|publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins|location=Philadelphia|isbn=978-0-7817-9079-6|page=419|url=http://books.google.ca/books?id=O9F7wtiPWxgC&pg=PA419|edition=5th}}</ref> |
|||
=== Alevlenme === |
|||
[[Kronik obstrüktif akciğer hastalığında akut alevlenme|Akut alevlenme]], KOAH hastası bireylerde görülen, artan nefes kesilmeleri, artan balgam üretimi, balgamın temizden yeşil/sarı renge dönmesi, öksürüklerin artması olarak tanımlanabilir.<ref name=EB2008/> Bu durum, yükselen soluk almanın [[bulgu]]larına da eşlik edebilir: [[takipne|hızlı nefes alma]], [[taşikardi|yüksek kalp hızı]], [[terleme]], etkin [[solunum kası]] kullanımı, [[siyanoz|derinin mavileşmesi]], [[konfüzyon]] veya ciddi alevlenmelerde görülen hırçın davranışlar.<ref name=EB2008>{{cite journal|last=Gruber|first=Phillip|title=The Acute Presentation of Chronic Obstructive Pulmonary Disease In the Emergency Department: A Challenging Oxymoron|journal=Emergency Medicine Practice|date=Kasım 2008|volume=10|issue=11|url=http://www.ebmedicine.net/topics.php?paction=showTopic&topic_id=63}}</ref><ref name=Burl2012>{{cite journal | author = Brulotte CA, Lang ES | title = Acute exacerbations of chronic obstructive pulmonary disease in the emergency department | journal = Emerg. Med. Clin. North Am. | volume = 30 | issue = 2 | pages = 223–47, vii |date=May 2012 | pmid = 22487106 | doi = 10.1016/j.emc.2011.10.005 }}</ref> Stetoskopla yapılan incelemelerde akciğer üstünden [[Ral (tıp)|ral]] duyulabilir.<ref>{{cite book|last=Spiro|first=Stephen|title=Clinical respiratory medicine expert consult|publisher=Saunders|location=Philadelphia, PA|isbn=978-1-4557-2329-4<!--|loc=Chapter 43-->|url=http://books.google.ca/books?id=2sOJk-yKPpUC&pg=PT2420|edition=4th |year=2012}}</ref> |
|||
== Nedenleri == |
== Nedenleri == |
||
The primary cause of COPD is tobacco smoke, with occupational exposure and pollution from indoor fires being significant causes in some countries.<ref name=GOLD2013Chp1/> Typically these exposures must occur over several decades before symptoms develop.<ref name=GOLD2013Chp1/> A person's genetic makeup also affects the risk.<ref name=GOLD2013Chp1/> |
|||
* Mesleki zararlı gazlar, tanecikler (mikro parçacık) solunması |
|||
* Etkin biçimde sigara kullanımı |
|||
* Hava kirliliği |
|||
* Genetik (alfa-1-antitripsin enzim eksikliği) |
|||
== |
=== Sigara === |
||
{{Multiple image|direction=vertical|align=right|image1=Female Smoking by Country.png|image2=Male Smoking by Country.png|width=250|caption1=Percentage of females smoking tobacco as of the late 1990s early 2000s|caption2=Percentage of males smoking tobacco as of the late 1990s early 2000s. Note the scales used for females and males differ.<ref name="isbn92-4-159628-7">{{cite book | author = World Health Organization | title = WHO Report on the Global Tobacco Epidemic 2008: The MPOWER Package | publisher = World Health Organization | location = Geneva | year = 2008 | isbn = 92-4-159628-7 | url = http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf |pages=268–309}}</ref>}} |
|||
* Öksürük |
|||
The primary risk factor for COPD globally is [[Smoking|tobacco smoking]].<ref name=GOLD2013Chp1/> Of those who smoke about 20% will get COPD,<ref name=Ward2012>{{cite book|last=Ward|first=Helen|title=Oxford Handbook of Epidemiology for Clinicians|year=2012|publisher=Oxford University Press|isbn=978-0-19-165478-7|pages=289–290|url=http://books.google.ca/books?id=dHLjLwru-l8C&pg=RA1-PT194#v=onepage&q&f=false}}</ref> and of those who are lifelong smokers about half will get COPD.<ref name=La2009>{{cite journal|last=Laniado-Laborín|first=R|title=Smoking and chronic obstructive pulmonary disease (COPD). Parallel epidemics of the 21st century|journal=International journal of environmental research and public health|date=January 2009|volume=6|issue=1|pages=209–24|pmid=19440278|doi=10.3390/ijerph6010209|pmc=2672326}}</ref> In the United States and United Kingdom, of those with COPD, 80-95% are either current smokers or previously smoked.<ref name=Ward2012/><ref name=Ren2013>{{cite book|last=Rennard|first=Stephen|title=Clinical management of chronic obstructive pulmonary disease|year=2013|publisher=Informa Healthcare|location=New York|isbn=978-0-8493-7588-0|page=23|url=http://books.google.ca/books?id=DiTThQJkc0UC&pg=PA23|edition=2nd}}</ref><ref name=Rich2010>{{cite book|author=Anita Sharma ; with a contribution by David Pitchforth ; forewords by Gail Richards|title=COPD in primary care|year=2010|publisher=Radcliffe Pub.|location=Oxford|isbn=978-1-84619-316-3|page=9|url=http://books.google.com/books?id=CrXFqhezbeMC&pg=PA9|author2=Barclay, Joyce}}</ref> The likelihood of developing COPD increases with the [[pack years|total smoke exposure]].<ref>{{cite book|last=Goldman|first=Lee|title=Goldman's Cecil medicine|publisher=Elsevier/Saunders|location=Philadelphia|isbn=978-1-4377-1604-7|page=537|url=http://books.google.ca/books?id=Qd-vvNh0ee0C&pg=PA537|edition=24th|year=2012}}</ref> Additionally, women are more susceptible to the harmful effects of smoke than men.<ref name=Rich2010/> In non-smokers, [[secondhand smoke]] is the cause of about 20% of cases.<ref name=Ren2013/> Other types of smoke, such as marijuana, cigar, and water pipe smoke, also confer a risk.<ref name=GOLD2013Chp1/> Women who smoke during [[pregnancy]] may increase the risk of COPD in their child.<ref name=GOLD2013Chp1/> |
|||
* Balgam çıkarma |
|||
* Kan tükürme |
|||
* Soluk darlığı |
|||
* Kanın oksijen doymuşluğunda azalma |
|||
* Kalp yetmezliğine bağlı, ayaklarda şişme |
|||
* Göğüste tıkanma |
|||
* Hırıltılı solunum |
|||
== |
=== Hava kirliliği === |
||
Poorly ventilated cooking fires, often fueled by coal or [[biomass fuel]]s such as wood and animal dung, lead to [[indoor air quality|indoor air pollution]] and are one of the most common causes of COPD in [[developing country|developing countries]].<ref name=Ken2007>{{cite journal |author=Kennedy SM, Chambers R, Du W, Dimich-Ward H|title=Environmental and occupational exposures: do they affect chronic obstructive pulmonary disease differently in women and men?|journal=Proceedings of the American Thoracic Society|volume=4 |issue=8 |pages=692–4 |date=December 2007|pmid=18073405 |url=http://pats.atsjournals.org/cgi/content/full/4/8/692 |doi=10.1513/pats.200707-094SD}}</ref> These fires are a method of cooking and heating for nearly 3 billion people with their health effects being greater among women due to more exposure.<ref name=GOLD2013Chp1/><ref name=Ken2007/> They are used as the main source of energy in 80% of homes in India, China and [[sub-Saharan Africa]].<ref name=Piro2012/> |
|||
[[Astım]], genellikle çocuk ve genç yaşlarda görülürken, KOAH, 50 yaşlarından sonra ortaya çıkar. KOAH sigara içenlerde görülmesine karşın, astımın sıgara ile ilgisi yoktur. Astımda iyileşme olanaklıyken, KOAH'ın sağaltımında (tedavisinde), akciğerde yaratılan hasarın geriye dönüşü yoktur. |
|||
People who live in large cities have a higher rate of COPD compared to people who live in rural areas.<ref>{{cite journal|author=Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM |title=Global burden of COPD: systematic review and meta-analysis |journal=Eur. Respir. J. |volume=28 |issue=3 |pages=523–32 |date=September 2006|pmid=16611654|doi=10.1183/09031936.06.00124605 }}</ref> While urban [[air pollution]] is a contributing factor in exacerbations, its overall role as a cause of COPD is unclear.<ref name=GOLD2013Chp1/> Areas with poor outdoor air quality, including that from [[exhaust gas]], generally have higher rates of COPD.<ref name=Piro2012/> The overall effect in relation to smoking, however, is believed to be small.<ref name=GOLD2013Chp1/> |
|||
{| class="wikitable" style="text-align:center;width:100%;" |
|||
=== Mesleki maruz === |
|||
Intense and prolonged exposure to workplace dusts, chemicals and fumes increase the risk of COPD in both smokers and nonsmokers.<ref name=Dev2006/> Workplace exposures are believed to be the cause in 10–20% of cases.<ref>{{cite book|last=Laine|first=Christine|title=In the Clinic: Practical Information about Common Health Problems|year=2009|publisher=ACP Press|isbn=978-1-934465-64-6|page=226|url=http://books.google.ca/books?id=bvg9he4FOB0C&pg=PA226}}</ref> In the United States they are believed to be related to more than 30% of cases among those who have never smoked and probably represent a greater risk in countries without sufficient regulations.<ref name=GOLD2013Chp1/> |
|||
A number of industries and sources have been implicated, including<ref name=Piro2012/> high levels of dust in [[coal mining]], [[gold mining]], and the cotton textile industry, occupations involving [[cadmium]] and [[isocyanates]], and fumes from [[welding]].<ref name=Dev2006>{{cite journal |doi=10.1136/bmj.332.7550.1142 |title=Definition, epidemiology and risk factors |year=2006 |last1=Devereux |first1=Graham |journal=BMJ |volume=332 |issue=7550 |pages=1142–4 |pmid=16690673 |pmc=1459603}}</ref> Working in agriculture is also a risk.<ref name=Piro2012/> In some professions the risks have been estimated as equivalent to that of half to two packs of cigarettes a day.<ref name=Barn2009/> [[Silica]] dust exposure can also lead to COPD, with the risk unrelated to that for [[silicosis]].<ref>{{cite journal |doi=10.1515/REVEH.2007.22.4.255 |title=Chronic Obstructive Pulmonary Disease and Occupational Exposure to Silica |year=2007 |last1=Rushton |first1=Lesley |journal=Reviews on Environmental Health |volume=22 |issue=4 |pmid=18351226 |pages=255–72}}</ref> The negative effects of dust exposure and cigarette smoke exposure appear to be additive or possibly more than additive.<ref name=Barn2009>{{cite book |displayeditors=4 |editor1-first=Peter J. |editor1-last=Barnes |editor2-first=Jeffrey M. |editor2-last=Drazen |editor3-first=Stephen I. |editor3-last=Rennard |editor4-first=Neil C. |editor4-last=Thomson |year=2009 |chapter=Relationship between cigarette smoking and occupational exposures |chapterurl=http://books.google.ca/books?id=HY9PiQL3kQMC&pg=PA464 |title=Asthma and COPD: Basic Mechanisms and Clinical Management |publisher=Academic |location=Amsterdam |isbn=978-0-12-374001-4 |page=464}}</ref> |
|||
=== Genetik === |
|||
Genetics play a role in the development of COPD.<ref name=GOLD2013Chp1/> It is more common among relatives of those with COPD who smoke than unrelated smokers.<ref name=GOLD2013Chp1/> Currently, the only clearly inherited risk factor is [[alpha 1-antitrypsin deficiency]] (AAT).<ref name=Foreman2012>{{cite journal | author = Foreman MG, Campos M, Celedón JC | title = Genes and chronic obstructive pulmonary disease | journal = Med. Clin. North Am. | volume = 96 | issue = 4 | pages = 699–711 |date=July 2012 | pmid = 22793939 | pmc = 3399759 | doi = 10.1016/j.mcna.2012.02.006 }}</ref> This risk is particularly high if someone deficient in [[alpha 1-antitrypsin]] also smokes.<ref name=Foreman2012/> It is responsible for about 1–5% of cases<ref name=Foreman2012/><ref name=Brode2012>{{cite journal | author = Brode SK, Ling SC, Chapman KR | title = Alpha-1 antitrypsin deficiency: a commonly overlooked cause of lung disease | journal = CMAJ | volume = 184 | issue = 12 | pages = 1365–71 |date=September 2012 | pmid = 22761482 | pmc = 3447047 | doi = 10.1503/cmaj.111749 }}</ref> and the condition is present in about 3–4 in 10,000 people.<ref name=Harr2012/> Other genetic factors are being investigated,<ref name=Foreman2012/> of which there are likely to be many.<ref name=Piro2012>{{cite journal | author = Pirozzi C, Scholand MB | title = Smoking cessation and environmental hygiene | journal = Med. Clin. North Am. | volume = 96 | issue = 4 | pages = 849–67 |date=July 2012 | pmid = 22793948 | doi = 10.1016/j.mcna.2012.04.014 }}</ref> |
|||
=== Diğer === |
|||
A number of other factors are less closely linked to COPD. The risk is greater in those who are poor, although it is not clear if this is due to [[poverty]] itself or other risk factors associated with poverty, such as air pollution and malnutrition.<ref name=GOLD2013Chp1/> There is tentative evidence that those with asthma and airway hyperreactivity are at increased risk of COPD.<ref name=GOLD2013Chp1/> Birth factors such as low birth weight may also play a role as do a number of infectious diseases including [[HIV/AIDS]] and [[tuberculosis]].<ref name=GOLD2013Chp1/> [[Respiratory infections]] such as [[pneumonia]] do not appear to increase the risk of COPD, at least in adults.<ref name=Harr2012/> |
|||
=== Ataklar === |
|||
An acute exacerbation (a sudden worsening of symptoms)<ref name=GOLD2013Chp5>{{cite book |last=Vestbo |first=Jørgen |title=Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease|year=2013|publisher=Global Initiative for Chronic Obstructive Lung Disease |chapter=Management of Exacerbations |pages=39–45 |chapterurl=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf#56}}</ref> is commonly triggered by infection or environmental pollutants, or sometimes by other factors such as improper use of medications.<ref name=Dhar2012>{{cite book|last=Dhar|first=Raja|title=Textbook of pulmonary and critical care medicine|year=2011|publisher=Jaypee Brothers Medical Publishers|location=New Delhi|isbn=978-93-5025-073-0|page=1056|url=http://books.google.ca/books?id=rAT1bdnDakAC&pg=PA1056}}</ref> Infections appear to be the cause of 50 to 75% of cases,<ref name=Dhar2012/><ref>{{cite book|last=Palange|first=Paolo|title=ERS Handbook of Respiratory Medicine|year=2013|publisher=European Respiratory Society|isbn=978-1-84984-041-5|page=194|url=http://books.google.ca/books?id=48gaALnXhcQC&pg=PA194}}</ref> with bacteria in 25%, viruses in 25%, and both in 25%.<ref>{{cite book|last=Lötvall|first=Jan|title=Advances in combination therapy for asthma and COPD|year=2011|publisher=John Wiley & Sons|location=Chichester, West Sussex|isbn=978-1-119-97846-6|page=251|url=http://books.google.ca/books?id=oPDU4xQLVWEC&pg=PT265}}</ref> Environmental pollutants include both poor indoor and outdoor air quality.<ref name=Dhar2012/> Exposure to personal smoke and secondhand smoke increases the risk.<ref name=Piro2012/> Cold temperature may also play a role, with exacerbations occurring more commonly in winter.<ref name=Barnes2009>{{cite book|last=Barnes|first=Peter|title=Asthma and COPD : basic mechanisms and clinical management|year=2009|publisher=Academic|location=Amsterdam|isbn=978-0-12-374001-4|page=837|url=http://books.google.ca/books?id=HY9PiQL3kQMC&pg=PA837|edition=2nd}}</ref> Those with more severe underlying disease have more frequent exacerbations: in mild disease 1.8 per year, moderate 2 to 3 per year, and severe 3.4 per year.<ref>{{cite book|last=Hanania|first=Nicola|title=COPD a Guide to Diagnosis and Clinical Management|publisher=Springer Science+Business Media, LLC|location=Totowa, NJ|isbn=978-1-59745-357-8|page=197|url=http://books.google.ca/books?id=wMzWnIdRD1MC&pg=PA197|edition=1st|date=2010-12-09}}</ref> Those with many exacerbations have a faster rate of deterioration of their lung function.<ref name=Beasley2012>{{cite journal|last=Beasley|first=V|author2=Joshi, PV |author3=Singanayagam, A |author4=Molyneaux, PL |author5=Johnston, SL |author6= Mallia, P |title=Lung microbiology and exacerbations in COPD|journal=International journal of chronic obstructive pulmonary disease|year=2012|volume=7|pages=555–69|pmid=22969296|doi=10.2147/COPD.S28286|pmc=3437812}}</ref> [[Pulmonary embolism|Pulmonary emboli]] (blood clots in the lungs) can worsen symptoms in those with pre-existing COPD.<ref name=Lancet2012/> |
|||
== Patofizyoloji == |
|||
[[File:Copd 2010Side.JPG|thumb|upright=2|On the left is a diagram of the lungs and airways with an inset showing a detailed cross-section of normal [[bronchiole]]s and [[alveoli]]. On the right is lungs damaged by COPD with an inset showing a cross-section of damaged bronchioles and alveoli]] |
|||
COPD is a type of [[obstructive lung disease]] in which chronic incompletely reversible poor airflow (airflow limitation) and inability to breathe out fully (air trapping) exist.<ref name=Lancet2012/> The poor airflow is the result of breakdown of lung tissue (known as emphysema) and small airways disease known as obstructive bronchiolitis.<!-- <ref name=GOLD2013Chp1/> --> The relative contributions of these two factors vary between people.<ref name=GOLD2013Chp1/> Severe destruction of small airways can lead to the formation of large air pockets—known as bullae—that replace lung tissue. This form of disease is called bullous emphysema.<ref name="Fishman">{{Cite book | author=Murphy DMF, Fishman AP | title=Fishman's Pulmonary Diseases and Disorders | publisher=McGraw-Hill | year=2008 | page=913 | chapter=Chapter 53 | edition=4th | isbn=0-07-145739-9 }}</ref> |
|||
[[File:Emphysema low mag.jpg|thumb|left|[[Micrograph]] showing emphysema (left - large empty spaces) and [[lung]] tissue with relative preservation of the alveoli (right).]] |
|||
<!--Lung destruction --> |
|||
COPD develops as a significant and chronic inflammatory response to inhaled irritants.<ref name=GOLD2013Chp1/> Chronic bacterial infections may also add to this inflammatory state.<ref name=Beasley2012/> The inflammatory cells involved include [[neutrophil granulocyte]]s and [[macrophage]]s, two types of white blood cell.<!-- <ref name=GOLD2013Chp1/> --> Those who smoke additionally have [[Cytotoxic T cell|Tc1]] [[lymphocyte]] involvement and some people with COPD have [[eosinophil granulocyte|eosinophil]] involvement similar to that in asthma.<!-- <ref name=GOLD2013Chp1/> --> Part of this cell response is brought on by inflammatory mediators such as [[chemotaxis|chemotactic factors]].<!-- <ref name=GOLD2013Chp1/> --> Other processes involved with lung damage include [[oxidative stress]] produced by high concentrations of [[Radical (chemistry)|free radicals]] in tobacco smoke and released by inflammatory cells, and breakdown of the [[connective tissue]] of the lungs by [[protease]]s that are insufficiently inhibited by [[Protease inhibitor (biology)|protease inhibitors]].<!-- <ref name=GOLD2013Chp1/> --> The destruction of the connective tissue of the lungs is what leads to emphysema, which then contributes to the poor airflow and, finally, poor absorption and release of respiratory gases.<ref name=GOLD2013Chp1/> General muscle wasting that often occurs in COPD may be partly due to inflammatory mediators released by the lungs into the blood.<ref name=GOLD2013Chp1/> |
|||
<!--Airway narrowing --> |
|||
Narrowing of the airways occurs due to inflammation and scarring within them.<!-- <ref name=GOLD2013Chp1/> --> This contributes to the inability to breathe out fully.<!-- <ref name=GOLD2013Chp1/> --> The greatest reduction in air flow occurs when breathing out, as the pressure in the chest is compressing the airways at this time.<ref name=Cal2005>{{cite journal |author=Calverley PM, Koulouris NG |title=Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology|journal=Eur Respir J |volume=25 |pages=186–199|year=2005|pmid=15640341 |doi=10.1183/09031936.04.00113204 |issue=1}}</ref> This can result in more air from the previous breath remaining within the lungs when the next breath is started, resulting in an increase in the total volume of air in the lungs at any given time, a process called [[Inhalation#Hyperaeration|hyperinflation]] or air trapping.<ref name=Cal2005/><ref>{{cite book|last=Currie|first=Graeme P.|title=ABC of COPD|year=2010|publisher=Wiley-Blackwell, BMJ Books|location=Chichester, West Sussex, UK|isbn=978-1-4443-2948-3|page=32|url=http://books.google.ca/books?id=eEoYQA4QD_wC&pg=PA32|edition=2nd }}</ref> Hyperinflation from exercise is linked to shortness of breath in COPD, as it is less comfortable to breathe in when the lungs are already partly full.<ref name=Odon2006>{{cite journal |author=O'Donnell DE|title=Hyperinflation, Dyspnea, and Exercise Intolerance in Chronic Obstructive Pulmonary Disease|journal=The Proceedings of the American Thoracic Society|volume=3 |pages=180–4 |year=2006 |pmid=16565429 |doi=10.1513/pats.200508-093DO |issue=2}}</ref> |
|||
Some also have a degree of [[Bronchial hyperresponsiveness|airway hyperresponsiveness]] to irritants similar to those found in asthma.<ref name=Harr2012/> |
|||
<!-- End stage --> |
|||
[[hypoxemia|Low oxygen levels]] and, eventually, [[hypercapnia|high carbon dioxide levels in the blood]] can occur from poor [[gas exchange]] due to decreased ventilation from airway obstruction, hyperinflation and a reduced desire to breathe.<ref name=GOLD2013Chp1/> During exacerbations, airway inflammation is also increased, resulting in increased hyperinflation, reduced expiratory airflow and worsening of gas transfer. This can also lead to insufficient ventilation and, eventually, low blood oxygen levels.<ref name=GOLD2007/> Low oxygen levels, if present for a prolonged period, can result in [[vasoconstriction|narrowing of the arteries]] in the lungs, while emphysema leads to breakdown of capillaries in the lungs.<!-- <ref name=GOLD2013Chp1/> --> Both these changes result in increased blood pressure in the [[Pulmonary artery|pulmonary arteries]], which may cause cor pulmonale.<ref name=GOLD2013Chp1/> |
|||
== Tanı == |
|||
[[File:DoingSpirometry.JPG|alt=A person sitting and blowing into a device attached to a computer|thumb|A person blowing into a spirometer. Smaller handheld devices are available for office use.]] |
|||
The diagnosis of COPD should be considered in anyone over the age of 35 to 40 who has [[dyspnea|shortness of breath]], a chronic cough, sputum production, or frequent winter colds and a history of exposure to risk factors for the disease.<ref name=GOLD2013Chp2/><ref name=NICE2010P60/> [[Spirometry]] is then used to confirm the diagnosis.<ref name=GOLD2013Chp2/><ref name=Qas2011/> |
|||
=== Spirometri === |
|||
[[Spirometry]] measures the amount of airflow obstruction present and is generally carried out after the use of a [[bronchodilator]], a medication to open up the airways.<ref name=Qas2011/> Two main components are measured to make the diagnosis: the forced expiratory volume in one second (FEV<sub>1</sub>), which is the greatest volume of air that can be breathed out in the first second of a breath, and the [[vital capacity|forced vital capacity]] (FVC), which is the greatest volume of air that can be breathed out in a single large breath.<ref name=Young2010>{{cite book|last=Young|first=Vincent B.|title=Blueprints medicine|year=2010|publisher=Wolters Kluwer Health/Lippincott William & Wilkins|location=Philadelphia|isbn=978-0-7817-8870-0|page=69|url=http://books.google.ca/books?id=_DHtahEUgXcC&pg=PA69|edition=5th}}</ref> Normally, 75–80% of the FVC comes out in the first second<ref name=Young2010/> and a [[FEV1/FVC ratio|FEV<sub>1</sub>/FVC ratio]] of less than 70% in someone with symptoms of COPD defines a person as having the disease.<ref name=Qas2011/> Based on these measurements, spirometry would lead to over-diagnosis of COPD in the elderly.<ref name=Qas2011/> The [[National Institute for Health and Care Excellence]] criteria additionally require a FEV<sub>1</sub> of less than 80% of predicted.<ref name=NICE2010P60/> |
|||
Evidence for using spirometry among those without symptoms in an effort to [[Screening (medicine)|diagnose the condition earlier]] is of uncertain effect and is therefore currently not recommended.<ref name=GOLD2013Chp2/><ref name=Qas2011>{{cite journal |doi=10.7326/0003-4819-155-3-201108020-00008 |title=Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease: A Clinical Practice Guideline Update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society |year=2011 |last1=Qaseem |first1=Amir |journal=Annals of Internal Medicine |volume=155 |issue=3 |pages=179–91 |pmid=21810710 |last2=Wilt |first2=TJ |last3=Weinberger |first3=SE |last4=Hanania |first4=NA |last5=Criner |first5=G |last6=Van Der Molen |first6=T |last7=Marciniuk |first7=DD |last8=Denberg |first8=T |last9=Schünemann |first9=H |last10=Wedzicha |first10=W |last11=MacDonald |first11=R |last12=Shekelle |first12=P |author13=American College Of Physicians |author14=American College of Chest Physicians |author15=American Thoracic Society |author16=European Respiratory Society |url=http://annals.org/article.aspx?articleid=479627}}</ref> A [[peak expiratory flow]] (the maximum speed of expiration), commonly used in asthma, is not sufficient for the diagnosis of COPD.<ref name=NICE2010P60/> |
|||
=== Şiddet === |
|||
{| class="wikitable" style = "float: right; margin-left:15px; text-align:center" |
|||
|+MRC shortness of breath scale<ref name=NICE2010P60/> |
|||
|- |
|- |
||
! Grade!! Activity affected |
|||
! Hastalığın ciddiyeti !! FEV<sub>1</sub> (beklenenin yüzdesi) |
|||
|- |
|- |
||
| 1 || Only strenuous activity |
|||
| Hafif || ≥80 |
|||
|- |
|- |
||
| |
| 2 || Vigorous walking |
||
|- |
|- |
||
| 3 || With normal walking |
|||
| Ağır || 30-49 |
|||
|- |
|- |
||
| 4 || After a few minutes of walking |
|||
| Çok ağır || <30 veya süreğen (kronik) solunum sıkıntısı belirtileri |
|||
|- |
|||
| 5 || With changing clothing |
|||
|} |
|||
{| class="wikitable" style = "float: right; margin-left:15px; text-align:center" |
|||
|+GOLD grade<ref name=GOLD2013Chp2/> |
|||
|- |
|||
! Severity!! FEV<sub>1</sub> % predicted |
|||
|- |
|||
| Mild (GOLD 1) || ≥80 |
|||
|- |
|||
| Moderate (GOLD 2)|| 50–79 |
|||
|- |
|||
| Severe (GOLD 3) || 30–49 |
|||
|- |
|||
| Very severe (GOLD 4)|| <30 or [[chronic respiratory failure]] |
|||
|} |
|} |
||
There are a number of methods to determine how much COPD is affecting a given individual.<ref name=GOLD2013Chp2/> The modified [[Medical Research Council (United Kingdom)|British Medical Research Council]] questionnaire (mMRC) or the COPD assessment test (CAT) are simple questionnaires that may be used to determine the severity of symptoms.<ref name=GOLD2013Chp2/> Scores on CAT range from 0–40 with the higher the score, the more severe the disease.<ref name=ATS>{{cite web |title=COPD Assessment Test (CAT) |url=http://www.thoracic.org/assemblies/srn/questionaires/copd.php |publisher=[[American Thoracic Society]] |accessdate=November 29, 2013}}</ref> Spirometry may help to determine the severity of airflow limitation.<ref name=GOLD2013Chp2/> This is typically based on the FEV<sub>1</sub> expressed as a percentage of the predicted "normal" for the person's age, gender, height and weight.<ref name=GOLD2013Chp2/> Both the American and European guidelines recommended partly basing treatment recommendations on the FEV<sub>1</sub>.<ref name=Qas2011/> The GOLD guidelines suggest dividing people into four categories based on symptoms assessment and airflow limitation.<ref name=GOLD2013Chp2/> Weight loss and muscle weakness, as well as the presence of other diseases, should also be taken into account.<ref name=GOLD2013Chp2/> |
|||
== Tanı == |
|||
Hastalığın tanısı, akciğer grafisi ve SFT (Solunum işlevi incelemesi)'nin yanı sıra [[EKG]] ve tam kan sayımı ile [[bilgisayarlı tomografi]] (BT) taramaları sonucu konulur. |
|||
== |
=== Diğer testler === |
||
A [[chest X-ray]] and [[complete blood count]] may be useful to exclude other conditions at the time of diagnosis.<ref name=NICE2010P70/> Characteristic signs on X-ray are overexpanded lungs, a flattened [[Thoracic diaphragm|diaphragm]], increased retrosternal airspace, and [[Bulla (dermatology)|bullae]] while it can help exclude other lung diseases, such as [[pneumonia]], [[pulmonary edema]] or a [[pneumothorax]].<ref name=Old2007>{{cite journal |author=Torres M, Moayedi S |title=Evaluation of the acutely dyspneic elderly patient |journal=Clin. Geriatr. Med. |volume=23 |issue=2 |pages=307–25, vi |date=May 2007 |pmid=17462519 |doi=10.1016/j.cger.2007.01.007}}</ref> A high-resolution [[X-ray computed tomography|computed tomography]] scan of the chest may show the distribution of emphysema throughout the lungs and can also be useful to exclude other lung diseases.<ref name=Harr2012/> Unless surgery is planned, however, this rarely affects management.<ref name=Harr2012/> An [[arterial blood gas|analysis of arterial blood]] is used to determine the need for oxygen; this is recommended in those with an FEV<sub>1</sub> less than 35% predicted, those with a peripheral oxygen saturation of less than 92% and those with symptoms of congestive heart failure.<ref name=GOLD2013Chp2/> In areas of the world where alpha-1 antitrypsin deficiency is common, people with COPD (particularly those below the age of 45 and with emphysema affecting the lower parts of the lungs) should be considered for testing.<ref name=GOLD2013Chp2/> |
|||
* A tipi ([[Amfizem]]) |
|||
* B tipi ([[bronşit]]) |
|||
* C tipi (karışık) |
|||
<gallery> |
|||
== Sağaltım (tedavi) == |
|||
File:COPD.JPG|alt=A black and white image, with a small white heart in the middle and large black lungs around it|Chest X-ray demonstrating severe COPD. Note the small heart size in comparison to the lungs. |
|||
Tanı konulduktan sonra KOAH'ın evrelendirilmesi sonucunda sigaranın bırakılmasının yanı sıra benzer risk etkenlerinin azaltılması yoluna gidilir. Kullanılacak ilaçlar [[astım]] tedavisinde olduğu gibi solunum yoluyla kullanılan püskürtülen ilaçlardır (spreyler). İlaç dışı sağaltımı için kanlarında Oksijen bölümsel basıncı hastalık nedeniyle belirli bir değerin altına düşmüş olgularda '''hekim kararıyla''' oksijen terapisi uygulanır. Öksürük ile balgam çıkarma olağandışı boyutlara varırsa (akut, iveğen atak), hastanın yatarak iyileştirilmesi söz konusudur. [[Fizyoterapi]], solunum alıştırmaları, beslenme desteği ve psiko-sosyal desteklerle yardımcı unsurlar kullanılır. Cerrahi yöntemler de uygulanmaktadır. |
|||
File:Barrowchest.JPG|A lateral chest x-ray of a person with emphysema. Note the barrel chest and flat diaphragm. |
|||
Image:BullaCXR.PNG|Lung bulla as seen on CXR in a person with severe COPD |
|||
Medical X-Ray imaging WFH07 nevit.jpg|A severe case of bullous emphysema |
|||
File:Bullus emphasemaCT.png|Axial CT image of the lung of a person with end-stage bullous emphysema. |
|||
</gallery> |
|||
=== Ayırıcı tanı === |
|||
COPD may need to be differentiated from other causes of shortness of breath such as [[congestive heart failure]], [[pulmonary embolism]], [[pneumonia]] or [[pneumothorax]]. Many people with COPD mistakenly think they have [[asthma]].<ref name=EB2008/> The distinction between asthma and COPD is made on the basis of the symptoms, smoking history, and whether airflow limitation is reversible with bronchodilators at [[spirometry]].<ref>{{cite web|author1=BTS COPD Consortium|title=Spirometry in practice - a practical guide to using spirometry in primary care |url=https://www.brit-thoracic.org.uk/document-library/delivery-of-respiratory-care/spirometry/spirometry-in-practice/|accessdate=25 August 2014|pages=8–9|year=2005}}</ref> Tuberculosis may also present with a chronic cough and should be considered in locations where it is common.<ref name=GOLD2013Chp2/> Less common conditions that may present similarly include [[bronchopulmonary dysplasia]] and [[obliterative bronchiolitis]].<ref name=NICE2010P70>{{NICE|101|Chronic Obstructive Pulmonary Disease|June 2010|70–80}}</ref> Chronic bronchitis may occur with normal airflow and in this situation it is not classified as COPD.<ref name=Harr2012/> |
|||
== Önlem == |
|||
Most cases of COPD are potentially preventable through decreasing exposure to smoke and improving air quality.<ref name=Piro2012/> Annual [[influenza vaccination]]s in those with COPD reduce exacerbations, hospitalizations and death.<ref name=Mackay2012>{{cite journal | author = Mackay AJ, Hurst JR | title = COPD exacerbations: causes, prevention, and treatment | journal = Med. Clin. North Am. | volume = 96 | issue = 4 | pages = 789–809 |date=July 2012 | pmid = 22793945 | doi = 10.1016/j.mcna.2012.02.008 }}</ref><ref>{{cite journal |author=Poole PJ, Chacko E, Wood-Baker RW, Cates CJ |title=Influenza vaccine for patients with chronic obstructive pulmonary disease |journal=Cochrane Database Syst Rev |volume=1 |pages=CD002733 |year=2006 |pmid=16437444|doi=10.1002/14651858.CD002733.pub2 |editor1-last=Poole |editor1-first=Phillippa}}</ref> [[Pneumococcal vaccine|Pneumococcal vaccination]] may also be beneficial.<ref name=Mackay2012/> |
|||
=== Sigarayı bırakma === |
|||
<!--Primary prevention --> |
|||
Keeping people from starting smoking is a key aspect of preventing COPD.<ref name=GOLD2013ChpX/> The [[Tobacco smoking#Legal issues and regulation|policies]] of governments, public health agencies and anti-smoking organizations can reduce smoking rates by discouraging people from starting and encouraging people to stop smoking.<ref name=WHO2003/> [[Smoking ban]]s in public areas and places of work are important measures to decrease exposure to secondhand smoke and while many places have instituted bans more are recommended.<ref name=Piro2012/> |
|||
<!--Secondary prevention --> |
|||
In those who smoke, [[smoking cessation|stopping smoking]] is the only measure shown to slow down the worsening of COPD.<ref name=Jim2013>{{cite journal | author = Jiménez-Ruiz CA, Fagerström KO | title = Smoking cessation treatment for COPD smokers: the role of counselling | journal = Monaldi Arch Chest Dis | volume = 79 | issue = 1 | pages = 33–7 |date=March 2013 | pmid = 23741944 }}</ref> Even at a late stage of the disease, it can reduce the rate of worsening lung function and delay the onset of disability and death.<ref name=kc>{{cite book |author=Kumar P, Clark M |title=Clinical Medicine |publisher=Elsevier Saunders |year=2005 |isbn=0-7020-2763-4 |pages=900–1 |edition=6th }}</ref> Smoking cessation starts with the decision to stop smoking, leading to an attempt at quitting. Often several attempts are required before long-term abstinence is achieved.<ref name = WHO2003>{{cite book |url=http://www.who.int/tobacco/resources/publications/tobacco_dependence/en/ |publisher=World Health Organization |title=Policy Recommendations for Smoking Cessation and Treatment of Tobacco Dependence |isbn=978-92-4-156240-9 | pages=15–40}}</ref> Attempts over 5 years lead to success in nearly 40% of people.<ref name=Ton2013/> |
|||
Some smokers can achieve long-term smoking cessation through willpower alone. Smoking, however, is highly addictive,<ref>{{cite web |url=http://www.nhs.uk/chq/Pages/2278.aspx?CategoryID=53&SubCategoryID=536 |title=Why is smoking addictive? |work=NHS Choices |date=December 29, 2011 |accessdate=November 29, 2013}}</ref> and many smokers need further support. The chance of quitting is improved with social support, engagement in a smoking cessation program and the use of medications such as [[nicotine replacement therapy]], [[bupropion]] or [[varenicline]].<ref name=WHO2003/><ref name=Ton2013>{{cite journal | author = Tønnesen P | title = Smoking cessation and COPD | journal = Eur Respir Rev | volume = 22 | issue = 127 | pages = 37–43 |date=March 2013 | pmid = 23457163 | doi = 10.1183/09059180.00007212 }}</ref> |
|||
=== Meslek sağlığı === |
|||
A number of measures have been taken to reduce the likelihood that workers in at-risk industries—such as coal mining, construction and stonemasonry—will develop COPD.<ref name=Piro2012/> Examples of these measures include: the creation of public policy,<ref name=Piro2012/> education of workers and management about the risks, promoting smoking cessation, [[disease surveillance|checking]] workers for early signs of COPD, use of [[respirator]]s, and dust control.<ref>{{cite book|last=Smith|first=Barbara K. Timby, Nancy E.|title=Essentials of nursing : care of adults and children|year=2005|publisher=Lippincott Williams & Wilkins|location=Philadelphia|isbn=978-0-7817-5098-1|page=338|url=http://books.google.ca/books?id=LJWDJMoStnMC&pg=PA338}}</ref><ref>{{cite book |editor2-last=Markowitz |editor1-first=William N. |editor1-last=Rom |editor2-first=Steven B.|title=Environmental and occupational medicine|year=2007|publisher=Wolters Kluwer/Lippincott Williams & Wilkins|location=Philadelphia|isbn=978-0-7817-6299-1|pages=521–2|url=http://books.google.ca/books?id=H4Sv9XY296oC&pg=PA521|edition=4th }}</ref> Effective dust control can be achieved by improving ventilation, using water sprays and by using mining techniques that minimize dust generation.<ref>{{cite web |url=http://www.hse.gov.uk/copd/casestudies/wetcut.htm |title=Wet cutting |publisher=[[Health and Safety Executive]] |accessdate=November 29, 2013}}</ref> If a worker develops COPD, further lung damage can be reduced by avoiding ongoing dust exposure, for example by changing the work role.<ref>{{cite book|last=George|first=Ronald B.|title=Chest medicine : essentials of pulmonary and critical care medicine|year=2005|publisher=Lippincott Williams & Wilkins|location=Philadelphia, PA|isbn=978-0-7817-5273-2|page=172|url=http://books.google.ca/books?id=ZzlX2zJMbdgC&pg=PA172|edition=5th }}</ref> |
|||
=== Hava kirliliği === |
|||
Both indoor and outdoor air quality can be improved, which may prevent COPD or slow the worsening of existing disease.<ref name=Piro2012/> This may be achieved by public policy efforts, cultural changes, and personal involvement.<ref name=GOLD2013Chp4>{{cite book |last=Vestbo |first=Jørgen |title=Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease|year=2013|publisher=Global Initiative for Chronic Obstructive Lung Disease |pages=31–8 |chapter=Management of Stable COPD |url=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf#48}}</ref> |
|||
<!--Outdoor air --> |
|||
A number of developed countries have successfully improved outdoor air quality through regulations.<!-- <ref name=Piro2012/> --> This has resulted in improvements in the lung function of their populations.<ref name=Piro2012/> Those with COPD may experience fewer symptoms if they stay indoors on days when outdoor air quality is poor.<ref name=GOLD2007/> |
|||
<!--Indoor air --> |
|||
One key effort is to reduce exposure to smoke from cooking and heating fuels through improved ventilation of homes and better stoves and chimneys.<ref name=GOLD2013Chp4/> Proper stoves may improve indoor air quality by 85%.<!-- <ref name=Piro2012/> --> Using alternative energy sources such as [[solar cooking]] and electrical heating is effective,<!-- <ref name=Piro2012/> --> as is using fuels such as kerosene or coal rather than biomass.<ref name=Piro2012/> |
|||
== Yönetim == |
|||
There is no known cure for COPD, but the symptoms are treatable and its progression can be delayed.<ref name=GOLD2013ChpX/> The major goals of management are to reduce risk factors, manage stable COPD, prevent and treat acute exacerbations, and manage associated illnesses.<ref name=GOLD2007/> The only measures that have been shown to reduce mortality are smoking cessation and supplemental oxygen.<ref name=Drummond08>{{cite journal |author=Drummond MB, Dasenbrook EC, Pitz MW, Murphy DJ, Fan E|title=Inhaled corticosteroids in patients with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis |journal=JAMA |volume=300 |issue=20 |pages=2407–16 |date=November 2008 |pmid=19033591|doi=10.1001/jama.2008.717 }}</ref> Stopping smoking decreases the risk of death by 18%.<ref name=Lancet2012/> Other recommendations include influenza vaccination once a year, pneumococcal vaccination once every 5 years, and reduction in exposure to environmental air pollution.<ref name=Lancet2012/> In those with advanced disease, [[palliative care]] may reduce symptoms, with morphine improving the feelings of shortness of breath.<ref name=Carl2012>{{cite journal |author=Carlucci A, Guerrieri A, Nava S |title=Palliative care in COPD patients: is it only an end-of-life issue? |journal=Eur Respir Rev |volume=21 |issue=126 |pages=347–54 |date=December 2012|pmid=23204123|doi=10.1183/09059180.00001512 }}</ref> [[Noninvasive ventilation]] may be used to support breathing.<ref name=Carl2012/> |
|||
=== Egzersiz === |
|||
[[Pulmonary rehabilitation]] is a program of exercise, disease management and counseling, coordinated to benefit the individual.<ref>{{cite web|url=http://www.nhlbi.nih.gov/health/dci/Diseases/Copd/Copd_Treatments.html |title=COPD — Treatment |publisher=U.S. National Heart Lung and Blood Institute |accessdate=2013-07-23}}</ref> In those who have had a recent exacerbation, pulmonary rehabilitation appears to improve the overall quality of life and the ability to exercise, and reduce mortality.<ref name=Puhan2011>{{cite journal |author=Puhan MA, Gimeno-Santos E, Scharplatz M, Troosters T, Walters EH, Steurer J |editor1-last=Puhan |editor1-first=Milo A |title=Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease |journal=Cochrane Database Syst Rev |issue=10 |pages=CD005305 |year=2011|pmid=21975749 |doi=10.1002/14651858.CD005305.pub3 }}</ref> It has also been shown to improve the sense of control a person has over their disease, as well as their emotions.<ref name=Lac2006>{{cite journal | author = Lacasse Y, Goldstein R, Lasserson TJ, Martin S | title = Pulmonary rehabilitation for chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | volume =4 | pages = CD003793 | year = 2006 | pmid = 17054186 | doi = 10.1002/14651858.CD003793.pub2 | editor1-last = Lacasse | editor1-first = Yves }}</ref> Breathing exercises in and of themselves appear to have a limited role.<ref name=Holland2012/> |
|||
Being either underweight or overweight can affect the symptoms, degree of disability and prognosis of COPD. People with COPD who are underweight can improve their breathing muscle strength by increasing their calorie intake.<ref name=GOLD2007/> When combined with regular exercise or a pulmonary rehabilitation program, this can lead to improvements in COPD symptoms. Supplemental nutrition may be useful in those who are [[malnutrition|malnourished]].<ref name=Ferr2012>{{cite journal|author=Ferreira IM, Brooks D, White J, Goldstein R |editor1-last=Ferreira|editor1-first=Ivone M |title=Nutritional supplementation for stable chronic obstructive pulmonary disease |journal=Cochrane Database Syst Rev |volume=12 |pages=CD000998 |year=2012 |pmid=23235577 |doi=10.1002/14651858.CD000998.pub3 }}</ref> |
|||
=== Bronkodilatörler === |
|||
Inhaled [[bronchodilator]]s are the primary medications used<ref name=Lancet2012/> and result in a small overall benefit.<ref name=VanD2013>{{cite journal | author = van Dijk WD, van den Bemt L, van Weel C | title = Megatrials for bronchodilators in chronic obstructive pulmonary disease (COPD) treatment: time to reflect | journal = J Am Board Fam Med | volume = 26 | issue = 2 | pages = 221–4 | year = 2013 | pmid = 23471939 | doi = 10.3122/jabfm.2013.02.110342}}</ref> There are two major types, [[Beta2-adrenergic agonist|β<sub>2</sub> agonists]] and [[anticholinergics]]; both exist in long-acting and short-acting forms. They reduce shortness of breath, wheeze and exercise limitation, resulting in an improved [[quality of life]].<ref name=Lies2002>{{cite journal |author=Liesker JJ, Wijkstra PJ, Ten Hacken NH, Koëter GH, Postma DS, Kerstjens HA |title=A systematic review of the effects of bronchodilators on exercise capacity in patients with COPD |journal=Chest |volume=121 |issue=2 |pages=597–608 |date=February 2002|pmid=11834677 |doi= 10.1378/chest.121.2.597 |url=http://journal.publications.chestnet.org/article.aspx?articleid=1080303}}</ref> It is unclear if they change the progression of the underlying disease.<ref name=Lancet2012/> |
|||
In those with mild disease, short-acting agents are recommended on an [[Pro re nata|as needed]] basis.<ref name=Lancet2012/> In those with more severe disease, long-acting agents are recommended.<ref name=Lancet2012/> If long-acting bronchodilators are insufficient, then inhaled corticosteroids are typically added.<ref name=Lancet2012/> With respect to long-acting agents, it is unclear if [[tiotropium]] (a long-acting anticholinergic) or [[long-acting beta agonist]]s (LABAs) are better, and it may be worth trying each and continuing the one that worked best.<ref name=Chong2012>{{cite journal | author = Chong J, Karner C, Poole P | title = Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | volume = 9 | pages = CD009157 | year = 2012 | pmid = 22972134 | doi = 10.1002/14651858.CD009157.pub2 | editor1-last = Chong | editor1-first = Jimmy }}</ref> Both types of agent appear to reduce the risk of acute exacerbations by 15–25%.<ref name=Lancet2012/> While both may be used at the same time, any benefit is of questionable significance.<ref name=Karner2012>{{cite journal | author = Karner C, Cates CJ | title = Long-acting beta(2)-agonist in addition to tiotropium versus either tiotropium or long-acting beta(2)-agonist alone for chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | volume = 4 | pages = CD008989 | year = 2012 | pmid = 22513969 | doi = 10.1002/14651858.CD008989.pub2 | editor1-last = Karner | editor1-first = Charlotta }}</ref> |
|||
<!--Beta agonists --> |
|||
There are several short-acting β<sub>2</sub> agonists available including [[salbutamol]] (Ventolin) and [[terbutaline]].<ref name=GOLD2013Chp3/> They provide some relief of symptoms for four to six hours.<ref name=GOLD2013Chp3/> Long-acting β<sub>2</sub> agonists such as [[salmeterol]] and [[formoterol]] are often used as maintenance therapy. Some feel the evidence of benefits is limited<ref name=Cave2011>{{Cite journal | last1 = Cave | first1 = AC. | last2 = Hurst | first2 = MM. | title = The use of long acting β₂-agonists, alone or in combination with inhaled corticosteroids, in chronic obstructive pulmonary disease (COPD): a risk-benefit analysis | journal = Pharmacol Ther | volume = 130 | issue = 2 | pages = 114–43 |date=May 2011 | doi = 10.1016/j.pharmthera.2010.12.008 | pmid = 21276815 }}</ref> while others view the evidence of benefit as established.<ref>{{cite journal|last=Spencer|first=S|author2=Karner, C |author3=Cates, CJ |author4= Evans, DJ |title=Inhaled corticosteroids versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease|journal=Cochrane Database Syst Rev|date=Dec 7, 2011|issue=12|pages=CD007033|pmid=22161409|doi=10.1002/14651858.CD007033.pub3|editor1-last=Spencer|editor1-first=Sally}}</ref><ref>{{cite journal|last=Wang|first=J|author2=Nie, B |author3=Xiong, W |author4= Xu, Y |title=Effect of long-acting beta-agonists on the frequency of COPD exacerbations: a meta-analysis|journal=Journal of clinical pharmacy and therapeutics|date=April 2012|volume=37|issue=2|pages=204–11|pmid=21740451|doi=10.1111/j.1365-2710.2011.01285.x}}</ref> Long-term use appears safe in COPD<ref name=Decr2013>{{cite journal | author = Decramer ML, Hanania NA, Lötvall JO, Yawn BP | title = The safety of long-acting β2-agonists in the treatment of stable chronic obstructive pulmonary disease | journal = Int J Chron Obstruct Pulmon Dis | volume = 8 | pages = 53–64 | year = 2013 | pmid = 23378756 | pmc = 3558319 | doi = 10.2147/COPD.S39018 }}</ref> with adverse effects include [[tremor|shakiness]] and [[Palpitation|heart palpitations]].<ref name=Lancet2012/> When used with inhaled steroids they increase the risk of pneumonia.<ref name=Lancet2012/> While steroids and LABAs may work better together,<ref name=Cave2011/> it is unclear if this slight benefit outweighs the increased risks.<ref>{{cite journal|last=Nannini|first=LJ|author2=Lasserson, TJ |author3=Poole, P |title=Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease|journal=Cochrane Database Syst Rev|date=Sep 12, 2012|volume=9|pages=CD006829|pmid=22972099|doi=10.1002/14651858.CD006829.pub2|editor1-last=Nannini|editor1-first=Luis Javier}}</ref> |
|||
<!--Anticholinergics --> |
|||
There are two main anticholinergics used in COPD, [[ipratropium]] and [[tiotropium]]. Ipratropium is a short-acting agent while tiotropium is long-acting. Tiotropium is associated with a decrease in exacerbations and improved quality of life,<ref name=Karner2012>{{cite journal | author = Karner C, Chong J, Poole P | title = Tiotropium versus placebo for chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | volume = 7 | pages = CD009285 | year = 2012 | pmid = 22786525 | doi = 10.1002/14651858.CD009285.pub2 | editor1-last = Karner | editor1-first = Charlotta }}</ref> and tiotropium provides those benefits better than ipratropium.<ref>{{cite journal |author=Cheyne L, Irvin-Sellers MJ, White J |editor1-last=Cheyne |editor1-first=Leanne |title=Tiotropium versus ipratropium bromide for chronic obstructive pulmonary disease |journal=Cochrane Database of Systematic Reviews |date=Sep 16, 2013 |issue=9 |pages=CD009552 |doi=10.1002/14651858.CD009552.pub2 |pmid=24043433 |volume=9}}</ref> It does not appear to affect mortality or the over all hospitalization rate.<ref>{{cite journal|last=Karner|first=C|author2=Chong, J |author3=Poole, P |title=Tiotropium versus placebo for chronic obstructive pulmonary disease|journal=Cochrane Database Syst Rev|date=Jul 11, 2012|volume=7|pages=CD009285|pmid=22786525|doi=10.1002/14651858.CD009285.pub2|editor1-last=Karner|editor1-first=Charlotta}}</ref> Anticholinergics can cause dry mouth and urinary tract symptoms.<ref name=Lancet2012/> They are also associated with increased risk of heart disease and stroke.<ref name=Singh2008>{{cite journal | author = Singh S, Loke YK, Furberg CD | title = Inhaled anticholinergics and risk of major adverse cardiovascular events in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis | journal = JAMA | volume = 300 | issue = 12 | pages = 1439–50 |date=September 2008 | pmid = 18812535 | doi = 10.1001/jama.300.12.1439 }}</ref><ref name=Singh2013>{{cite journal | author = Singh S, Loke YK, Enright P, Furberg CD | title = Pro-arrhythmic and pro-ischaemic effects of inhaled anticholinergic medications | journal = Thorax | volume = 68 | issue = 1 | pages = 114–6 |date=January 2013 | pmid = 22764216 | doi = 10.1136/thoraxjnl-2011-201275 }}</ref> [[Aclidinium]], another long acting agent which came to market in 2012, has been used as an alternative to tiotropium.<ref>{{cite journal|last1=Jones|first1=P|title=Aclidinium bromide twice daily for the treatment of chronic obstructive pulmonary disease: a review.|journal=Advances in therapy|date=Apr 2013|volume=30|issue=4|pages=354–68|pmid=23553509|doi=10.1007/s12325-013-0019-2}}</ref><ref>{{cite journal|last1=Cazzola|first1=M|last2=Page|first2=CP|last3=Matera|first3=MG|title=Aclidinium bromide for the treatment of chronic obstructive pulmonary disease.|journal=Expert opinion on pharmacotherapy|date=Jun 2013|volume=14|issue=9|pages=1205–14|pmid=23566013|doi=10.1517/14656566.2013.789021}}</ref> |
|||
=== Kortikosteroitler === |
|||
[[Corticosteroid]]s are usually used in inhaled form but may also be used as tablets to treat and prevent acute exacerbations. While inhaled corticosteroids (ICS) have not shown benefit for people with mild COPD, they decrease acute exacerbations in those with either moderate or severe disease.<ref>{{cite journal |author=Gartlehner G, Hansen RA, Carson SS, Lohr KN |title=Efficacy and Safety of Inhaled Corticosteroids in Patients With COPD: A Systematic Review and Meta-Analysis of Health Outcomes |journal=Ann Fam Med |volume=4 |issue=3 |pages=253–62 |year=2006 |pmid=16735528 |pmc=1479432|doi=10.1370/afm.517 }}</ref> When used in combination with a LABA they decrease mortality more than either ICS or LABA alone.<ref name=Shaf2013>{{cite journal | author = Shafazand S | title = ACP Journal Club. Review: inhaled medications vary substantively in their effects on mortality in COPD | journal = Ann. Intern. Med. | volume = 158 | issue = 12 | pages = JC2 |date=June 2013 | pmid = 23778926 | doi = 10.7326/0003-4819-158-12-201306180-02002 }}</ref> By themselves they have no effect on overall one-year mortality and are associated with increased rates of pneumonia.<ref name="Drummond08"/> It is unclear if they affect the progression of the disease.<ref name=Lancet2012/> Long-term treatment with steroid tablets is associated with significant side effects.<ref name=GOLD2013Chp3/> |
|||
=== Diğer ilaçlar === |
|||
Long-term [[antibiotic]]s, specifically those from the [[macrolide]] class such as [[erythromycin]], reduce the frequency of exacerbations in those who have two or more a year.<ref name=Mammen2012>{{cite journal | author = Mammen MJ, Sethi S | title = Macrolide therapy for the prevention of acute exacerbations in chronic obstructive pulmonary disease | journal = Pol. Arch. Med. Wewn. | volume = 122 | issue = 1–2 | pages = 54–9 | year = 2012 | pmid = 22353707}}</ref><ref name=Harath2013>{{cite journal|last=Herath|first=SC|author2=Poole, P|title=Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD).|journal=Cochrane Database Syst Rev|date=Nov 28, 2013|volume=11|pages=CD009764|pmid=24288145|doi=10.1002/14651858.CD009764.pub2}}</ref> This practice may be cost effective in some areas of the world.<ref>{{cite journal|last=Simoens|first=S|author2=Laekeman, G |author3=Decramer, M |title=Preventing COPD exacerbations with macrolides: a review and budget impact analysis|journal=Respiratory medicine|date=May 2013|volume=107|issue=5|pages=637–48|pmid=23352223|doi=10.1016/j.rmed.2012.12.019}}</ref> Concerns include that of [[antibiotic resistance]] and hearing problems with [[azithromycin]].<ref name=Harath2013/> [[Xanthine|Methylxanthines]] such as [[theophylline]] generally cause more harm than benefit and thus are usually not recommended,<ref name=Bar2003>{{cite journal |author=Barr RG, Rowe BH, Camargo CA |editor1-last=Barr |editor1-first=R Graham |title=Methylxanthines for exacerbations of chronic obstructive pulmonary disease |journal=Cochrane Database Syst Rev |issue=2 |pages=CD002168 |year=2003 |pmid=12804425 |doi=10.1002/14651858.CD002168 }}</ref> but may be used as a second-line agent in those not controlled by other measures.<ref name=GOLD2007/> [[Mucolytic]]s may be useful in some people who have very thick mucus but are generally not needed.<ref name=Mackay2012/> [[Cough medicine]]s are not recommended.<ref name=GOLD2013Chp3/> |
|||
=== Oksijen === |
|||
[[Oxygen therapy|Supplemental oxygen]] is recommended in those with low oxygen levels at rest (a [[partial pressure of oxygen]] of less than 50–55 mmHg or oxygen saturations of less than 88%).<ref name=GOLD2013Chp3>{{cite book |last=Vestbo |first=Jørgen |title=Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease |year=2013 |publisher=Global Initiative for Chronic Obstructive Lung Disease |pages=19–30 |chapter=Therapeutic Options |chapterurl=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf#36}}</ref><ref name=Group2012/> In this group of people it decreases the risk of [[heart failure]] and death if used 15 hours per day<ref name=GOLD2013Chp3/><ref name=Group2012>{{cite journal|last=COPD Working|first=Group|title=Long-term oxygen therapy for patients with chronic obstructive pulmonary disease (COPD): an evidence-based analysis|journal=Ontario health technology assessment series|year=2012|volume=12|issue=7|pages=1–64|pmid=23074435|pmc=3384376}}</ref> and may improve people's ability to exercise.<ref name=Brad2005>{{cite journal | author = Bradley JM, O'Neill B | title = Short-term ambulatory oxygen for chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | volume =4 | pages = CD004356 | year = 2005 | pmid = 16235359 | doi = 10.1002/14651858.CD004356.pub3 | editor1-last = Bradley | editor1-first = Judy M }}</ref> In those with normal or mildly low oxygen levels, oxygen supplementation may improve shortness of breath.<ref name=Uron2011>{{cite journal | author = Uronis H, McCrory DC, Samsa G, Currow D, Abernethy A | title = Symptomatic oxygen for non-hypoxaemic chronic obstructive pulmonary disease | journal = Cochrane Database Syst Rev | issue = 6 | pages = CD006429 | year = 2011 | pmid = 21678356 | doi = 10.1002/14651858.CD006429.pub2 | editor1-last = Abernethy | editor1-first = Amy }}</ref> There is a risk of fires and little benefit when those on oxygen continue to smoke.<ref>{{cite book|last=Chapman|first=Stephen|title=Oxford handbook of respiratory medicine|year=2009|publisher=Oxford University Press|location=Oxford|isbn=978-0-19-954516-2|page=707|url=http://books.google.ca/books?id=945lM1g_uQoC&pg=PA707|edition=2nd}}</ref> In this situation some recommend against its use.<ref>{{cite book|last=Blackler|first=Laura|title=Managing chronic obstructive pulmonary disease|year=2007|publisher=John Wiley & Sons|location=Chichester, England|isbn=978-0-470-51798-7|page=49|url=http://books.google.ca/books?id=D5n6lqqxkNUC&pg=PA49}}</ref> During acute exacerbations, many require oxygen therapy; the use of high concentrations of oxygen without taking into account a person's oxygen saturations may lead to increased levels of carbon dioxide and worsened outcomes.<ref>{{cite book|last=Jindal|first=Surinder K|title=Chronic Obstructive Pulmonary Disease|year=2013|publisher=Jaypee Brothers Medical |isbn=978-93-5090-353-7|page=139|url=http://books.google.ca/books?id=PTgIAQAAQBAJ&pg=PA139}}</ref><ref name=BTS2008>{{cite journal|last=O'Driscoll|first=BR|last2=Howard |first2=LS |last3=Davison |first3=AG |author4=British Thoracic, Society|title=BTS guideline for emergency oxygen use in adult patients|journal=Thorax|date=October 2008|volume=63 |issue=Suppl 6|pages=vi1–68|pmid=18838559|doi=10.1136/thx.2008.102947}}</ref> In those at high risk of high carbon dioxide levels, oxygen saturations of 88–92% are recommended, while for those without this risk recommended levels are 94–98%.<ref name=BTS2008/> |
|||
=== Cerrahi === |
|||
For those with very severe disease surgery is sometimes helpful and may include [[lung transplantation]] or [[lung volume reduction surgery]].<ref name=Lancet2012/> Lung volume reduction surgery involves removing the parts of the lung most damaged by emphysema allowing the remaining, relatively good lung to expand and work better.<ref name=GOLD2013Chp3/> [[Lung transplantation]] is sometimes performed for very severe COPD, particularly in younger individuals.<ref name=GOLD2013Chp3/> |
|||
=== Ataklar === |
|||
Acute exacerbations are typically treated by increasing the usage of short-acting bronchodilators.<ref name=Lancet2012/> This commonly includes a combination of a short-acting inhaled beta agonist and anticholinergic.<ref name=GOLD2013Chp5/> These medications can be given either via a [[metered-dose inhaler]] with a [[Asthma spacer|spacer]] or via a [[nebulizer]] with both appearing to be equally effective.<ref name=GOLD2013Chp5/> Nebulization may be easier for those who are more unwell.<ref name=GOLD2013Chp5/> |
|||
Oral corticosteroids improve the chance of recovery and decrease the overall duration of symptoms.<ref name=Lancet2012/><ref name=GOLD2013Chp5/> They work equally well as intravenous steroids but appear to have fewer side effects.<ref>{{cite journal |last1=Walters |first1=JA |last2=Tan |first2=DJ |last3=White |first3=CJ |last4=Gibson |first4=PG |last5=Wood-Baker |first5=R |last6=Walters |first6=EH |title=Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease |journal=Cochrane Database Syst Rev |date=September 2014 |volume=9 |pages=CD001288 |pmid=25178099 |doi=10.1002/14651858.CD001288.pub4 |url=http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001288.pub4/abstract}}</ref> Five days of steroids work as well as ten or fourteen.<ref>{{cite journal|last1=Walters|first1=JA|last2=Tan|first2=DJ|last3=White|first3=CJ|last4=Wood-Baker|first4=R|title=Different durations of corticosteroid therapy for exacerbations of chronic obstructive pulmonary disease.|journal=The Cochrane database of systematic reviews|date=10 December 2014|volume=12|pages=CD006897|pmid=25491891}}</ref> In those with a severe exacerbation, antibiotics improve outcomes.<ref name=Vollen2012>{{cite journal |author=Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA |editor1-last=Vollenweider |editor1-first=Daniela J|title=Antibiotics for exacerbations of chronic obstructive pulmonary disease |journal=Cochrane Database Syst Rev |volume=12 |pages=CD010257 |year=2012 |pmid=23235687 |doi=10.1002/14651858.CD010257 }}</ref> A number of different antibiotics may be used including [[amoxicillin]], [[doxycycline]] and [[azithromycin]]; it is unclear if one is better than the others.<ref name=Mackay2012/> There is no clear evidence for those with less severe cases.<ref name=Vollen2012 /> |
|||
For those with [[respiratory failure|type 2 respiratory failure]] (acutely raised {{CO2}} levels) [[non-invasive positive pressure ventilation]] decreases the probability of death or the need of intensive care admission.<ref name=Lancet2012 /> Additionally, [[theophylline]] may have a role in those who do not respond to other measures.<ref name=Lancet2012 /> Fewer than 20% of exacerbations require hospital admission.<ref name=GOLD2013Chp5 /> In those without acidosis from respiratory failure, [[home care]] ("hospital at home") may be able to help avoid some admissions.<ref name=GOLD2013Chp5 /><ref>{{cite journal|last=Jeppesen|first=E|author2=Brurberg, KG |author3=Vist, GE |author4=Wedzicha, JA |author5=Wright, JJ |author6=Greenstone, M |author7= Walters, JA |title=Hospital at home for acute exacerbations of chronic obstructive pulmonary disease.|journal=Cochrane Database Syst Rev|date=May 16, 2012|volume=5|pages=CD003573|pmid=22592692 | doi=10.1002/14651858.CD003573.pub2}}</ref> |
|||
== Prognoz == |
|||
[[File:Chronic obstructive pulmonary disease world map - DALY - WHO2004.svg|250px|thumb|[[Disability-adjusted life year]] for chronic obstructive pulmonary disease per 100,000 inhabitants in 2004.<ref>{{cite web|url=http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html |title=WHO Disease and injury country estimates |year=2009 |work=World Health Organization |accessdate=Nov 11, 2009}}</ref> |
|||
{{Multicol}} |
|||
{{legend|#b3b3b3|no data}} |
|||
{{legend|#ffff65|≤110}} |
|||
{{legend|#fff200|110–220}} |
|||
{{legend|#ffdc00|220–330}} |
|||
{{legend|#ffc600|330–440}} |
|||
{{legend|#ffb000|440–550}} |
|||
{{legend|#ff9a00|550–660}} |
|||
{{Multicol-break}} |
|||
{{legend|#ff8400|660–770}} |
|||
{{legend|#ff6e00|770–880}} |
|||
{{legend|#ff5800|880–990}} |
|||
{{legend|#ff4200|990–1100}} |
|||
{{legend|#ff2c00|1100–1350}} |
|||
{{legend|#cb0000|≥1350}} |
|||
{{Multicol-end}}]] |
|||
COPD usually gets gradually worse over time and can ultimately result in death. It is estimated that 3% of [[disability adjusted life years|all disability]] is related to COPD.<ref name=DALY2012/> The proportion of disability from COPD globally has decreased from 1990 to 2010 due to improved indoor air quality primarily in Asia.<ref name=DALY2012>{{cite journal | author = Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, et al. | title = Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 | journal = Lancet | volume = 380 | issue = 9859 | pages = 2197–223 |date=December 2012 | pmid = 23245608 | doi = 10.1016/S0140-6736(12)61689-4 }}</ref> The overall number of years lived with disability from COPD, however, has increased.<ref name=YLD2012>{{cite journal | author = Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, et al. | title = Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 | journal = Lancet | volume = 380 | issue = 9859 | pages = 2163–96 |date=December 2012 | pmid = 23245607 | doi = 10.1016/S0140-6736(12)61729-2 }}</ref> |
|||
The rate at which COPD worsens varies with the presence of factors that predict a poor outcome, including severe airflow obstruction, little ability to exercise, shortness of breath, significantly underweight or overweight, [[congestive heart failure]], continued smoking, and frequent exacerbations.<ref name=GOLD2007/> Long-term outcomes in COPD can be estimated using the [[BODE index]] which gives a score of zero to ten depending on FEV<sub>1</sub>, [[body-mass index]], the distance walked in six minutes, and the [[modified MRC dyspnea scale]].<ref>{{cite book|last=Medicine|first=prepared by the Department of Medicine, Washington University School of|title=The Washington manual general internal medicine subspecialty consult.|year=2009|publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins|location=Philadelphia|isbn=978-0-7817-9155-7|page=96|url=http://books.google.ca/books?id=ZptEP_hDrlwC&pg=PA96|edition=2nd }}</ref> Significant weight loss is a bad sign.<ref name=Harr2012/> Results of spirometry are also a good predictor of the future progress of the disease but not as good as the BODE index.<ref name=Harr2012/><ref name=NICE2010P60/> |
|||
== Epidemiyoloji == |
|||
Globally, as of 2010, COPD affected approximately 329 million people (4.8% of the population) and is slightly more common in men than women.<ref name=YLD2012/> This is as compared to 64 million being affected in 2004.<ref>{{cite web|title=Chronic obstructive pulmonary disease (COPD) Fact sheet N°315|url=http://www.who.int/mediacentre/factsheets/fs315/en/|publisher=WHO|date=November 2012}}</ref> The increase in the developing world between 1970 and the 2000s is believed to be related to increasing rates of smoking in this region, an increasing population and an aging population due to less deaths from other causes such as infectious diseases.<ref name=Lancet2012/> Some developed countries have seen increased rates, some have remained stable and some have seen a decrease in COPD prevalence.<ref name=Lancet2012/> The global numbers are expected to continue increasing as risk factors remain common and the population continues to get older.<ref name=GOLD2013ChpX>{{cite book |last=Vestbo |first=Jørgen |title=Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease|year=2013|publisher=Global Initiative for Chronic Obstructive Lung Disease|pages=xiii–xv |nopp=yes |chapter=Introduction |url=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf#14}}</ref> |
|||
Between 1990 and 2010 the number of deaths from COPD decreased slightly from 3.1 million to 2.9 million<ref name=Lozano2012>{{cite journal | author = Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, et al.| title = Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010 | journal = Lancet | volume = 380 | issue = 9859 | pages = 2095–128 |date=December 2012 | pmid = 23245604 | doi = 10.1016/S0140-6736(12)61728-0 }}</ref> and became the fourth leading cause of death.<ref name=Lancet2012/> In 2012 it became the third leading cause as the number of deaths rose again to 3.1 million.<ref name="WHOTTCD" /> In some countries, mortality has decreased in men but increased in women.<ref name=Ryc2012>{{cite journal | author = Rycroft CE, Heyes A, Lanza L, Becker K | title = Epidemiology of chronic obstructive pulmonary disease: a literature review | journal = Int J Chron Obstruct Pulmon Dis | volume = 7 | pages = 457–94 | year = 2012 | pmid = 22927753 | pmc = 3422122 | doi = 10.2147/COPD.S32330 }}</ref> This is most likely due to rates of smoking in women and men becoming more similar.<ref name=Harr2012/> COPD is more common in older people;<ref name=GOLD2013Chp1/> it affects 34-200 out of 1000 people older than 65 years, depending on the population under review.<ref name=GOLD2013Chp1/><ref name="Old2007"/> |
|||
In England, an estimated 0.84 million people (of 50 million) have a diagnosis of COPD; this translates into approximately one person in 59 receiving a diagnosis of COPD at some point in their lives. In the most socioeconomically deprived parts of the country, one in 32 people were diagnosed with COPD, compared with one in 98 in the most affluent areas.<ref name="BJGPref">{{cite journal |author=Simpson CR, Hippisley-Cox J, Sheikh A| title= Trends in the epidemiology of chronic obstructive pulmonary disease in England: a national study of 51 804 patients | journal=Brit J Gen Pract |volume=60 |issue=576 |pages=483–8 |year=2010 |pmid=20594429 |pmc=2894402 |doi= 10.3399/bjgp10X514729}}</ref> In the United States approximately 6.3% of the adult population, totaling approximately 15 million people, have been diagnosed with COPD.<ref>{{cite journal |author=Centers for Disease Control and Prevention |title=Chronic Obstructive Pulmonary Disease Among Adults — United States, 2011 |journal=Morbidity and Mortality Weekly Report |date=Nov 23, 2012 |volume=61 |issue=46 |pages=938–43 |pmid=23169314 |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6146a2.htm}}</ref> 25 million people may have COPD if currently undiagnosed cases are included.<ref>{{cite web |title=Morbidity & Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases |publisher=National Heart, Lung, and Blood Institute |url=http://www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf |format=PDF}}</ref> In 2011, there were approximately 730,000 hospitalizations in the United States for COPD.<ref name=Tor2013>{{cite journal | author = Torio CM, Andrews RM | title = National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011: Statistical Brief #160 | journal = Healthcare Cost and Utilization Project (HCUP) Statistical Briefs| year = 2006| pmid = 24199255 | url = http://hcup-us.ahrq.gov/reports/statbriefs/sb160.jsp | publisher = Agency for Health Care Policy and Research }}</ref> |
|||
== Tarih == |
|||
[[File:Giambattista morgagni.gif|thumb|[[Giovanni Battista Morgagni]], who made one of the earliest recorded descriptions of emphysema in 1769]] |
|||
The word "emphysema" is derived from the [[Greek language|Greek]] {{lang|el|ἐμφυσᾶν}} ''emphysan'' meaning "''inflate''" -itself composed of ἐν ''en'', meaning "''in''", and φυσᾶν ''physan'', meaning "''breath, blast''{{-"}}.<ref>{{cite web|title=Emphysema|url=http://dictionary.reference.com/browse/emphysema|work=Dictionary.com|accessdate=21 November 2013}}</ref> The term chronic bronchitis came into use in 1808<ref name=History1991>{{cite journal |doi=10.1159/000195969 |title=History of the Treatment of Chronic Bronchitis |year=1991 |last1=Ziment |first1=Irwin |journal=Respiration |volume=58 |issue=Suppl 1 |pages=37–42 |pmid=1925077}}</ref> while the term COPD is believed to have first been used in 1965.<ref name=History2006/> Previously it has been known by a number of different names, including chronic obstructive bronchopulmonary disease, chronic obstructive respiratory disease, chronic airflow obstruction, chronic airflow limitation, chronic obstructive lung disease, nonspecific chronic pulmonary disease, and diffuse obstructive pulmonary syndrome.<!-- <ref name=History2006/> --> The terms chronic bronchitis and emphysema were formally defined in 1959 at the [[Novartis|CIBA]] guest symposium and in 1962 at the [[American Thoracic Society]] Committee meeting on Diagnostic Standards.<ref name=History2006/> |
|||
Early descriptions of probable emphysema include: in 1679 by T. Bonet of a condition of "voluminous lungs" and in 1769 by [[Giovanni Morgagni]] of lungs which were "turgid particularly from air".<ref name=History2006>{{cite journal |author=Petty TL |title=The history of COPD |journal=Int J Chron Obstruct Pulmon Dis |volume=1 |issue=1 |pages=3–14 |year=2006 |pmid=18046898 |pmc=2706597 |doi=10.2147/copd.2006.1.1.3}}</ref><ref name=Fish2008/> In 1721 the first drawings of emphysema were made by Ruysh.<ref name=Fish2008>{{cite book |first1=Joanne L. |last1=Wright |first2=Andrew |last2=Churg |chapter=Pathologic Features of Chronic Obstructive Pulmonary Disease: Diagnostic Criteria and Differential Diagnosis |chapterurl=http://www.mhprofessional.com/downloads/products/0071457399/0071457399_chap40.pdf |pages=693–705 |editor1-first=Alfred |editor1-last=Fishman |editor2-first=Jack |editor2-last=Elias |editor3-first=Jay |editor3-last=Fishman |editor4-first=Michael |editor4-last=Grippi |editor5-first=Robert |editor5-last=Senior |editor6-first=Allan |editor6-last=Pack |year=2008 |title=Fishman's Pulmonary Diseases and Disorders |edition=4th |publisher=McGraw-Hill |location=New York |isbn=978-0-07-164109-8}}</ref> These were followed with pictures by [[Matthew Baillie]] in 1789 and descriptions of the destructive nature of the condition.<!-- <ref name=History2006/> --> In 1814 [[Charles Badham (physician)|Charles Badham]] used "catarrh" to describe the cough and excess mucus in chronic bronchitis.<!-- <ref name=History2006/> --> [[René Laennec]], the physician who invented the [[stethoscope]], used the term "emphysema" in his book ''A Treatise on the Diseases of the Chest and of Mediate Auscultation'' (1837) to describe lungs that did not collapse when he opened the chest during an autopsy.<!-- <ref name=History2006/> --> He noted that they did not collapse as usual because they were full of air and the airways were filled with mucus.<!-- <ref name=History2006/> --> In 1842, [[John Hutchinson (surgeon)|John Hutchinson]] invented the [[spirometer]], which allowed the measurement of [[vital capacity]] of the lungs.<!-- <ref name=History2006/> --> However, his spirometer could only measure volume, not airflow.<!-- <ref name=History2006/> --> Tiffeneau and Pinelli in 1947 described the principles of measuring airflow.<ref name=History2006/> |
|||
In 1953, Dr. [[George Waldbott|George L. Waldbott]], an American allergist, first described a new disease he named "smoker's respiratory syndrome" in the 1953 ''Journal of the American Medical Association''. This was the first association between tobacco smoking and chronic respiratory disease.<ref>{{cite book|author1=George L. Waldbott|title=A struggle with Titans|date=1965|publisher=Carlton Press|page=6|url=http://books.google.com/books?id=hLRpAAAAMAAJ&q}}</ref> |
|||
Early treatments included garlic, cinnamon and [[ipecac]], among others.<ref name=History1991/> Modern treatments were developed during the second half of the 20th century.<!-- <ref name=History2005> --> Evidence supporting the use of [[steroid]]s in COPD were published in the late 1950s.<!-- <ref name=History2005> --> [[Bronchodilator]]s came into use in the 1960s following a promising trial of [[isoprenaline]].<!-- <ref name=History2005> --> Further bronchodilators, such as [[salbutamol]], were developed in the 1970s, and the use of [[LABA]]s began in the mid-1990s.<ref name=History2005>{{cite journal |author=Fishman AP |title=One hundred years of chronic obstructive pulmonary disease |journal=Am. J. Respir. Crit. Care Med. |volume=171 |issue=9 |pages=941–8|date=May 2005 |pmid=15849329 |doi=10.1164/rccm.200412-1685OE}}</ref> |
|||
== Toplum ve kültür == |
|||
{{See also|COPD Awareness Month}} |
|||
COPD has been referred to as "smoker's lung".<ref>{{cite book|last=Yuh-Chin|first=T. Huang|title=A clinical guide to occupational and environmental lung diseases|publisher=Humana Press|location=[New York]|isbn=978-1-62703-149-3|page=266|url=http://books.google.ca/books?id=9bYbE87FbtMC&pg=PA266|date=2012-10-28}}</ref> Those with emphysema have been known as "pink puffers" or "type A" due to their frequent pink complexion, fast respiratory rate and pursed lips,<ref>{{cite web|url=http://medical-dictionary.thefreedictionary.com/Pink+Puffer |title=Pink Puffer - definition of Pink Puffer in the Medical dictionary - by the Free Online Medical Dictionary, Thesaurus and Encyclopedia|publisher=Medical-dictionary.thefreedictionary.com |accessdate=2013-07-23}}</ref><ref name=Wein2013>{{cite book|last=Weinberger|first=Steven E.|title=Principles of pulmonary medicine|publisher=Elsevier/Saunders|location=Philadelphia|isbn=978-1-62703-149-3|page=165|url=http://books.google.ca/books?id=2F-DPG0c5IMC&pg=PT165|edition=6th|date=2013-05-08}}</ref> and people with chronic bronchitis have been referred to as "blue bloaters" or "type B" due to the often [[cyanosis|bluish color of the skin and lips]] from low oxygen levels and their ankle swelling.<ref name=Wein2013/><ref>{{cite book|last=Des Jardins|first=Terry|title=Clinical Manifestations & Assessment of Respiratory Disease|year=2013|publisher=Elsevier Health Sciences|isbn=978-0-323-27749-5|page=176|url=http://books.google.ca/books?id=LVtPAQAAQBAJ&pg=PA170|edition=6th}}</ref> This terminology is no longer accepted as useful as most people with COPD have a combination of both.<ref name=Harr2012/><ref name=Wein2013/> |
|||
Many health systems have difficulty ensuring appropriate identification, diagnosis and care of people with COPD; Britain's [[Department of Health (United Kingdom)|Department of Health]] has identified this as a major issue for the [[National Health Service (England)|National Health Service]] and has introduced a specific strategy to tackle these problems.<ref>{{cite book |url=https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216139/dh_128428.pdf |title=An outcomes strategy for people with chronic obstructive pulmonary disease (COPD) and asthma in England |date=18 July 2011 |publisher=[[Department of Health (United Kingdom)|Department of Health]]|page=5|accessdate=27 November 2013}}</ref> |
|||
=== Ekonomi === |
|||
Globally, as of 2010, COPD is estimated to result in economic costs of $2.1 trillion, half of which occurring in the developing world.<ref name=Cost2013/> Of this total an estimated $1.9 trillion are direct costs such as medical care, while $0.2 trillion are indirect costs such as missed work.<ref>{{cite book|last=Bloom|first=D|title=The Global Economic Burden of Noncommunicable Diseases|year=2011|publisher=World Economic Forum|page=24|url=http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf}}</ref> This is expected to more than double by the year 2030.<ref name=Cost2013/> In Europe, COPD represents 3% of healthcare spending.<ref name=GOLD2013Chp1/> In the United States, costs of the disease are estimated at $50 billion, most of which is due to exacerbation.<ref name=GOLD2013Chp1/> COPD was among the most expensive conditions seen in U.S. hospitals in 2011, with a total cost of about $5.7 billion.<ref name=Tor2013/> |
|||
== Araştırma == |
|||
{{See also|COPD: Journal of Chronic Obstructive Pulmonary Disease}} |
|||
[[Infliximab]], an immune-suppressing antibody, has been tested in COPD but there was no evidence of benefit with the possibility of harm.<ref>{{cite book|last=Nici|first=Linda|title=Chronic Obstructive Pulmonary Disease: Co-Morbidities and Systemic Consequences|year=2011|publisher=Springer|isbn=978-1-60761-673-3|page=78|url=http://books.google.ca/books?id=0CXcUnr-0eoC&pg=PA78}}</ref> [[Roflumilast]] shows promise in decreasing the rate of exacerbations but does not appear to change quality of life.<ref name=Lancet2012/> A number of new, long-acting agents are under development.<ref name=Lancet2012/> Treatment with [[stem cell]]s is under study,<ref>{{cite journal|last=Inamdar|first=AC|author2=Inamdar, AA|title=Mesenchymal stem cell therapy in lung disorders: pathogenesis of lung diseases and mechanism of action of mesenchymal stem cell.|journal=Experimental lung research|date=Oct 2013|volume=39|issue=8|pages=315–27|pmid=23992090|doi=10.3109/01902148.2013.816803}}</ref> and while generally safe and with promising animal data there is little human data as of 2014.<ref>{{cite journal|last=Conese|first=M|author2=Piro, D |author3=Carbone, A |author4=Castellani, S |author5= Di Gioia, S |title=Hematopoietic and mesenchymal stem cells for the treatment of chronic respiratory diseases: role of plasticity and heterogeneity.|journal=TheScientificWorldJournal|date=2014|volume=2014|pages=859817|pmid=24563632 |doi=10.1155/2014/859817 |pmc=3916026}}</ref> |
|||
== Diğer hayvanlar == |
|||
Chronic obstructive pulmonary disease may occur in a number of other animals and may be caused by exposure to tobacco smoke.<ref>{{cite book|last=Akers|first=R. Michael|title=Anatomy and Physiology of Domestic Animals|year=2008|publisher=Wiley|location=Arnes, AI|isbn=978-1-118-70115-7|page=852|url=http://books.google.ca/books?id=Ze6J2znDg38C&pg=PT852|author2=Denbow, D. Michael}}</ref><ref>{{cite journal|last=Wright|first=JL|author2=Churg, A|title=Animal models of cigarette smoke-induced COPD|journal=Chest|date=December 2002|volume=122|issue=6 Suppl|pages=301S–6S|pmid=12475805|doi=10.1378/chest.122.6_suppl.301S}}</ref> Most cases of the disease, however, are relatively mild.<ref>{{cite journal|last=Churg|first=A|author2=Wright, JL|title=Animal models of cigarette smoke-induced chronic obstructive lung disease|journal=Contributions to microbiology|year=2007|volume=14|pages=113–25|pmid=17684336|doi=10.1159/000107058|series=Contributions to Microbiology|isbn=3-8055-8332-X}}</ref> In [[horse]]s it is also known as [[recurrent airway obstruction]] and is typically due to an allergic reaction to a [[Mold|fungus]] contained in straw.<ref name=Marin2007>{{cite journal | author = Marinkovic D, Aleksic-Kovacevic S, Plamenac P | title = Cellular basis of chronic obstructive pulmonary disease in horses | journal = Int. Rev. Cytol. | volume = 257 | pages = 213–47 | year = 2007 | pmid = 17280899 | doi = 10.1016/S0074-7696(07)57006-3 | series = International Review of Cytology | isbn=978-0-12-373701-4 }}</ref> COPD is also commonly found in old dogs.<ref name=Miller1989>{{cite journal | author = Miller MS, Tilley LP, Smith FW | title = Cardiopulmonary disease in the geriatric dog and cat | journal = Vet. Clin. North Am. Small Anim. Pract. | volume = 19 | issue = 1 | pages = 87–102 |date=January 1989 | pmid = 2646821 }}</ref> |
|||
== Ayrıca bakınız == |
== Ayrıca bakınız == |
||
| 76. satır: | 275. satır: | ||
* [[Solunum]] |
* [[Solunum]] |
||
== |
== Bibliyografi == |
||
*{{cite web |url=http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf |title= Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease, Updated 2013|publisher=Global Initiative for Chronic Obstructive Lung Disease |accessdate=November 29, 2013}} |
|||
{{commonscat|Chronic obstructive pulmonary disease}} |
|||
*{{NICE|101|Chronic Obstructive Pulmonary Disease|June 2010|1-673}} |
|||
*{{cite journal |doi=10.7326/0003-4819-155-3-201108020-00008 |title=Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease: A Clinical Practice Guideline Update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society |year=2011 |last1=Qaseem |first1=Amir |journal=Annals of Internal Medicine |volume=155 |issue=3 |pages=179–91 |pmid=21810710 |last2=Wilt |first2=TJ |last3=Weinberger |first3=SE |last4=Hanania |first4=NA |last5=Criner |first5=G |last6=Van Der Molen |first6=T |last7=Marciniuk |first7=DD |last8=Denberg |first8=T |last9=Schünemann |first9=H |last10=Wedzicha |first10=W |last11=MacDonald |first11=R |last12=Shekelle |first12=P |author13=American College Of Physicians |author14=American College of Chest Physicians |author15=American Thoracic Society |author16=European Respiratory Society |url=http://annals.org/article.aspx?articleid=479627}} |
|||
== Dış bağlantılar == |
|||
{{commons category|Chronic obstructive pulmonary disease}} |
|||
*{{dmoz|Health/Conditions_and_Diseases/Respiratory_Disorders/Chronic_Obstructive_Pulmonary_Disease/}} |
|||
* [http://www.toraks.org.tr/sub/rehkoah.php Türk Toraks Derneği] |
* [http://www.toraks.org.tr/sub/rehkoah.php Türk Toraks Derneği] |
||
{{DEFAULTSORT:Chronic Obstructive Pulmonary Disease}} |
|||
{{hastalık-taslak}} |
|||
{{commonscat|Chronic obstructive pulmonary disease}} |
|||
== Kaynakça == |
|||
{{Reflist|30em}} |
|||
[[Kategori:Akciğer hastalıkları]] |
[[Kategori:Akciğer hastalıkları]] |
||
[[Kategori:Göğüs hastalıkları]] |
[[Kategori:Göğüs hastalıkları]] |
||
[[Kategori:Solunum sistemi hastalıkları]] |
[[Kategori:Solunum sistemi hastalıkları]] |
||
[[Kategori:Yaşa bağlı hastalıklar]] |
|||
[[Kategori:Meslek hastalıkları]] |
|||
[[Kategori:Tütün zehirlenmesi]] |
|||
Sayfanın 10.13, 2 Mart 2015 tarihindeki hâli
Bu sayfada devam eden bir çalışma vardır. Yardım etmek istiyorsanız ya da çalışma yarım bırakılmışsa, çalışmayı yapan kişilerle iletişime geçebilirsiniz. Bu sayfada son yedi gün içinde değişiklik yapılmadığı takdirde şablon sayfadan kaldırılacaktır. En son değişiklik, 9 yıl önce Bercaio (katkılar | kayıtlar) tarafından gerçekleştirildi (). |
| Kronik obstrüktif akciğer hastalığı | |
|---|---|
 | |
| Sigara içme durumunda tipik olarak görülen santrilobüler tip amfizemde, akciğerin gros patolojisi. Bu kesilmiş fiksajın yakından görünümünde, boşluklara dolmuş yoğun noktasal siyah karbon tortuları görülmektedir. | |
| Uzmanlık | Göğüs hastalıkları |
Kronik obstrüktif akciğer hastalığı (KOAH), zayıf hava akışının görüldüğü obstrüktif bir akciğer hastalığıdır. Tipik olarak zamanla daha kötüleşir. Ana belirtileri nefes darlığı, öksürme ve balgam üretimidir.[1] Kronik bronşit sahibi insanların çoğu aynı zamanda KOAH hastasıdır.[2]
Tütün içiciliği hastalığın en temel nedeni olup hava kirliliği ve genetik gibi daha az etkili nedenleri de vardır.[3] Gelişmekte olan ülkelerde, hava kirliliğinin en etkili nedenlerinden biri doğru havalandırılmamış yemek pişirme ve ısıtma ateşi dumanıdır. Bu tahriş edici şeylere uzun süreli maruz kalmalar, akciğerlerde iltihaplanmaya neden olarak küçük hava yollarının daralmasına ve amfizem adı verilen doku parçalanmasına yol açar.[4] Teşhis, zayıf hava akışını kontrol eden akciğer fonksiyon testleri ile anlaşılır.[5] Astımdan farklı olarak, KOAH hastalarında hava akışı herhangi bir ilaç yardımıyla belirgin bir şekilde düzelemez.
KOAH, bilinen nedenlere maruz kalınımı düşürerek önlenebilir. Bunlar arasında sigara içme oranlarını azaltmak ve iç/dış hava kalitesini yükseltmek gösterilebilir. KOAH tedavileri sigarayı bırakma, aşılar, rehabilitasyon, sıkça içe çekilen bronkodilatörler ve steroitler içerir. Bazı insanlar, uzun süreli oksijen terapisi veya akciğer nakliyle belirgin iyileşmeler gösterebilir.[4] Akut kötüleşme periyotları gösteren hastalarda, artan oranlarda ilaç ve hastane altında gözetim gerekebilir.
Dünya çapında KOAH, 329 milyon insanı (dünya nüfusunun %5'i) etkilemektedir. 2012'de 3 milyon insanın ölümüne sebebiyet vererek, dünyadaki en ölümcül üçüncü hastalık olarak tanımlandı.[6] Ölümlerin, yükselen sigara kullanımı ve bazı ülkelerdeki yaşlanan nüfus nedeniyle daha da artacağı öngörülmektedir.[7] 2010'da hastalığın 2.1 trilyon dolarlık bir ekonomik zarara yol açtığı tahmin edildi.[8]
Belirtiler ve semptomlar
 |
|
| Dinlerken sorun mu yaşıyorsunuz? Medya yardımı alın. | |
KOAH'ın en belirgin belirtisi balgam üretimi, nefes darlığı ve sık öksürmelerdir.[9] Bu belirtiler, uzun sürelere yayılmış bir şekilde görülür[2] ve tipik olarak zamanla kötüleşir.[4] KOAH'ın farklı tiplerinin olup olmadığı kesinleştirilmiş değildir.[3] Önceden amfizem ve kronik bronşit olarak ayrılan hastalıkta, amfizem aslında bir hastalıktan ziyade akciğerdeki değişimleri belirtmek adına kullanılır. Kronik bronşit ise, KOAH hastalığına eşlik edip etmeyeceği kesin olmayan, sadece bazı belirtileri açıklayan bir terimdir.[1]
Öksürme
Kronik öksürmeler gözlenebilen ilk belirtilerdir. İki yıldan uzun bir sürede, yılda üç aydan fazla süren ve balgam üretiminin eşlik ettiği durum, fazladan herhangi bir açıklama yapılmadığı sürece kronik bronşit tanımına dahil olur. Bu durum, KOAH tamamen başlamadan önce de görülebilir. Üretilen balgam miktarı, saatler veya günler arasında farklılık gösterebilir. Bazı durumlarda, öksürük görülmeyebilir ve sıklıkla gözlenmeyen bir biçimde rastlanılabilir. Bazı insanlar bu belirtileri sigaraya atfederler. Balgam, toplumsal ve kültürel koşullara göre yutulup tükürülebilir. Kuvvetli öksürmeler kaburga kırılması veya kısa süreli bilinç kaybına sebebiyet verebilir. KOAH tanısı konulan insanların genelde uzun süren "nezle" geçmişleri vardır.[9]
Nefes kesilmesi
Nefes darlığı hastaların en çok şikayet ettiği belirtidir.[10] Bu durum sıklıkla şöyle tanımlanır: "zorlukla nefes alıyorum", "nefesim kesiliyor" veya "yeterince hava alamıyorum".[11] Ancak farklı terimler farklı kültürlerde kullanılabilir.[9] Tipik olarak nefes darlığı, uzun süreli güç harcama durumlarında daha kötü bir hal alır ve zamanla kötüleşir.[9] İleri vakalarda dinlenme sırasında da gözlenebilir ve sürekli gözlenebilir.[12][13] Bu durum, KOAH hastalarının endişe duyduğu ve hayat kalitesini düşüren en başlıca belirtidir.[9] Daha ileri düzey KOAH hastaları büzülmüş dudaklarından nefes alır ve bu bazı durumlarda nefes darlığını iyileştirebilir.[14][15]
Diğer özellikler
KOAH hastalarında nefes vermek nefes almaktan uzun sürebilir[16] Göğüs sıkışması görülebilir[9] ancak çok yaygın değildir ve başka bir durumdan dolayı kaynaklanabilir.[10] Nefes yolları engellenmiş hastalar hırıldayabilir veya nefes alırken stetoskoba daha az ses verebilir.[16] Fıçı göğüs de KOAH hastalığının karakteristik belirtisidir ancak görece daha az rastlanır.[16] Tripod pozisyonu hastalık kötüleştikçe gözlenebilir.[2]
İleri düzey KOAH, akciğer arterlerinde yüksek basınca neden olabilir ve bu nedenle kalbin sağ karıncığına baskı uygulayabilir.[4][17][18] Cor pulmonale olarak adlandırılan bu durum, bacak şişmesine [9] ve şişen boyun damarına neden olabilir.[4] KOAH, diğer bütün akciğer hastalıklarından daha büyük bir cor pulmonale tetikleyicisidir.[17] Ancak, cor pulmonale, oksijen tedavisinin kullanımından beri daha az yaygındır.[2]
KOAH, daha çok paylaşılan risk faktörleri nedeniyle, diğer bazı durumlarla beraber gerçekleşir.[3] Bunlar arasında koroner arter hastalığı, yüksek kan basıncı, diyabet, kas yıkımı, osteoporoz, akciğer kanseri, anksiyete bozukluğu ve depresyon yer alır.[3] Ciddi hastalıkları olan insanlarda hâlsizlik yaygın görülür.[9] Çomak parmak, KOAH'ya özgü değildir ve altta yatan bir akciğer kanseri için araştırmaları tetiklemelidir.[19]
Alevlenme
Akut alevlenme, KOAH hastası bireylerde görülen, artan nefes kesilmeleri, artan balgam üretimi, balgamın temizden yeşil/sarı renge dönmesi, öksürüklerin artması olarak tanımlanabilir.[16] Bu durum, yükselen soluk almanın bulgularına da eşlik edebilir: hızlı nefes alma, yüksek kalp hızı, terleme, etkin solunum kası kullanımı, derinin mavileşmesi, konfüzyon veya ciddi alevlenmelerde görülen hırçın davranışlar.[16][20] Stetoskopla yapılan incelemelerde akciğer üstünden ral duyulabilir.[21]
Nedenleri
The primary cause of COPD is tobacco smoke, with occupational exposure and pollution from indoor fires being significant causes in some countries.[1] Typically these exposures must occur over several decades before symptoms develop.[1] A person's genetic makeup also affects the risk.[1]
Sigara
The primary risk factor for COPD globally is tobacco smoking.[1] Of those who smoke about 20% will get COPD,[23] and of those who are lifelong smokers about half will get COPD.[24] In the United States and United Kingdom, of those with COPD, 80-95% are either current smokers or previously smoked.[23][25][26] The likelihood of developing COPD increases with the total smoke exposure.[27] Additionally, women are more susceptible to the harmful effects of smoke than men.[26] In non-smokers, secondhand smoke is the cause of about 20% of cases.[25] Other types of smoke, such as marijuana, cigar, and water pipe smoke, also confer a risk.[1] Women who smoke during pregnancy may increase the risk of COPD in their child.[1]
Hava kirliliği
Poorly ventilated cooking fires, often fueled by coal or biomass fuels such as wood and animal dung, lead to indoor air pollution and are one of the most common causes of COPD in developing countries.[28] These fires are a method of cooking and heating for nearly 3 billion people with their health effects being greater among women due to more exposure.[1][28] They are used as the main source of energy in 80% of homes in India, China and sub-Saharan Africa.[29]
People who live in large cities have a higher rate of COPD compared to people who live in rural areas.[30] While urban air pollution is a contributing factor in exacerbations, its overall role as a cause of COPD is unclear.[1] Areas with poor outdoor air quality, including that from exhaust gas, generally have higher rates of COPD.[29] The overall effect in relation to smoking, however, is believed to be small.[1]
Mesleki maruz
Intense and prolonged exposure to workplace dusts, chemicals and fumes increase the risk of COPD in both smokers and nonsmokers.[31] Workplace exposures are believed to be the cause in 10–20% of cases.[32] In the United States they are believed to be related to more than 30% of cases among those who have never smoked and probably represent a greater risk in countries without sufficient regulations.[1]
A number of industries and sources have been implicated, including[29] high levels of dust in coal mining, gold mining, and the cotton textile industry, occupations involving cadmium and isocyanates, and fumes from welding.[31] Working in agriculture is also a risk.[29] In some professions the risks have been estimated as equivalent to that of half to two packs of cigarettes a day.[33] Silica dust exposure can also lead to COPD, with the risk unrelated to that for silicosis.[34] The negative effects of dust exposure and cigarette smoke exposure appear to be additive or possibly more than additive.[33]
Genetik
Genetics play a role in the development of COPD.[1] It is more common among relatives of those with COPD who smoke than unrelated smokers.[1] Currently, the only clearly inherited risk factor is alpha 1-antitrypsin deficiency (AAT).[35] This risk is particularly high if someone deficient in alpha 1-antitrypsin also smokes.[35] It is responsible for about 1–5% of cases[35][36] and the condition is present in about 3–4 in 10,000 people.[2] Other genetic factors are being investigated,[35] of which there are likely to be many.[29]
Diğer
A number of other factors are less closely linked to COPD. The risk is greater in those who are poor, although it is not clear if this is due to poverty itself or other risk factors associated with poverty, such as air pollution and malnutrition.[1] There is tentative evidence that those with asthma and airway hyperreactivity are at increased risk of COPD.[1] Birth factors such as low birth weight may also play a role as do a number of infectious diseases including HIV/AIDS and tuberculosis.[1] Respiratory infections such as pneumonia do not appear to increase the risk of COPD, at least in adults.[2]
Ataklar
An acute exacerbation (a sudden worsening of symptoms)[37] is commonly triggered by infection or environmental pollutants, or sometimes by other factors such as improper use of medications.[38] Infections appear to be the cause of 50 to 75% of cases,[38][39] with bacteria in 25%, viruses in 25%, and both in 25%.[40] Environmental pollutants include both poor indoor and outdoor air quality.[38] Exposure to personal smoke and secondhand smoke increases the risk.[29] Cold temperature may also play a role, with exacerbations occurring more commonly in winter.[41] Those with more severe underlying disease have more frequent exacerbations: in mild disease 1.8 per year, moderate 2 to 3 per year, and severe 3.4 per year.[42] Those with many exacerbations have a faster rate of deterioration of their lung function.[43] Pulmonary emboli (blood clots in the lungs) can worsen symptoms in those with pre-existing COPD.[3]
Patofizyoloji

COPD is a type of obstructive lung disease in which chronic incompletely reversible poor airflow (airflow limitation) and inability to breathe out fully (air trapping) exist.[3] The poor airflow is the result of breakdown of lung tissue (known as emphysema) and small airways disease known as obstructive bronchiolitis. The relative contributions of these two factors vary between people.[1] Severe destruction of small airways can lead to the formation of large air pockets—known as bullae—that replace lung tissue. This form of disease is called bullous emphysema.[44]
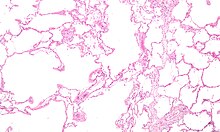
COPD develops as a significant and chronic inflammatory response to inhaled irritants.[1] Chronic bacterial infections may also add to this inflammatory state.[43] The inflammatory cells involved include neutrophil granulocytes and macrophages, two types of white blood cell. Those who smoke additionally have Tc1 lymphocyte involvement and some people with COPD have eosinophil involvement similar to that in asthma. Part of this cell response is brought on by inflammatory mediators such as chemotactic factors. Other processes involved with lung damage include oxidative stress produced by high concentrations of free radicals in tobacco smoke and released by inflammatory cells, and breakdown of the connective tissue of the lungs by proteases that are insufficiently inhibited by protease inhibitors. The destruction of the connective tissue of the lungs is what leads to emphysema, which then contributes to the poor airflow and, finally, poor absorption and release of respiratory gases.[1] General muscle wasting that often occurs in COPD may be partly due to inflammatory mediators released by the lungs into the blood.[1]
Narrowing of the airways occurs due to inflammation and scarring within them. This contributes to the inability to breathe out fully. The greatest reduction in air flow occurs when breathing out, as the pressure in the chest is compressing the airways at this time.[45] This can result in more air from the previous breath remaining within the lungs when the next breath is started, resulting in an increase in the total volume of air in the lungs at any given time, a process called hyperinflation or air trapping.[45][46] Hyperinflation from exercise is linked to shortness of breath in COPD, as it is less comfortable to breathe in when the lungs are already partly full.[47]
Some also have a degree of airway hyperresponsiveness to irritants similar to those found in asthma.[2]
Low oxygen levels and, eventually, high carbon dioxide levels in the blood can occur from poor gas exchange due to decreased ventilation from airway obstruction, hyperinflation and a reduced desire to breathe.[1] During exacerbations, airway inflammation is also increased, resulting in increased hyperinflation, reduced expiratory airflow and worsening of gas transfer. This can also lead to insufficient ventilation and, eventually, low blood oxygen levels.[4] Low oxygen levels, if present for a prolonged period, can result in narrowing of the arteries in the lungs, while emphysema leads to breakdown of capillaries in the lungs. Both these changes result in increased blood pressure in the pulmonary arteries, which may cause cor pulmonale.[1]
Tanı

The diagnosis of COPD should be considered in anyone over the age of 35 to 40 who has shortness of breath, a chronic cough, sputum production, or frequent winter colds and a history of exposure to risk factors for the disease.[9][10] Spirometry is then used to confirm the diagnosis.[9][48]
Spirometri
Spirometry measures the amount of airflow obstruction present and is generally carried out after the use of a bronchodilator, a medication to open up the airways.[48] Two main components are measured to make the diagnosis: the forced expiratory volume in one second (FEV1), which is the greatest volume of air that can be breathed out in the first second of a breath, and the forced vital capacity (FVC), which is the greatest volume of air that can be breathed out in a single large breath.[49] Normally, 75–80% of the FVC comes out in the first second[49] and a FEV1/FVC ratio of less than 70% in someone with symptoms of COPD defines a person as having the disease.[48] Based on these measurements, spirometry would lead to over-diagnosis of COPD in the elderly.[48] The National Institute for Health and Care Excellence criteria additionally require a FEV1 of less than 80% of predicted.[10]
Evidence for using spirometry among those without symptoms in an effort to diagnose the condition earlier is of uncertain effect and is therefore currently not recommended.[9][48] A peak expiratory flow (the maximum speed of expiration), commonly used in asthma, is not sufficient for the diagnosis of COPD.[10]
Şiddet
| Grade | Activity affected |
|---|---|
| 1 | Only strenuous activity |
| 2 | Vigorous walking |
| 3 | With normal walking |
| 4 | After a few minutes of walking |
| 5 | With changing clothing |
| Severity | FEV1 % predicted |
|---|---|
| Mild (GOLD 1) | ≥80 |
| Moderate (GOLD 2) | 50–79 |
| Severe (GOLD 3) | 30–49 |
| Very severe (GOLD 4) | <30 or chronic respiratory failure |
There are a number of methods to determine how much COPD is affecting a given individual.[9] The modified British Medical Research Council questionnaire (mMRC) or the COPD assessment test (CAT) are simple questionnaires that may be used to determine the severity of symptoms.[9] Scores on CAT range from 0–40 with the higher the score, the more severe the disease.[50] Spirometry may help to determine the severity of airflow limitation.[9] This is typically based on the FEV1 expressed as a percentage of the predicted "normal" for the person's age, gender, height and weight.[9] Both the American and European guidelines recommended partly basing treatment recommendations on the FEV1.[48] The GOLD guidelines suggest dividing people into four categories based on symptoms assessment and airflow limitation.[9] Weight loss and muscle weakness, as well as the presence of other diseases, should also be taken into account.[9]
Diğer testler
A chest X-ray and complete blood count may be useful to exclude other conditions at the time of diagnosis.[51] Characteristic signs on X-ray are overexpanded lungs, a flattened diaphragm, increased retrosternal airspace, and bullae while it can help exclude other lung diseases, such as pneumonia, pulmonary edema or a pneumothorax.[52] A high-resolution computed tomography scan of the chest may show the distribution of emphysema throughout the lungs and can also be useful to exclude other lung diseases.[2] Unless surgery is planned, however, this rarely affects management.[2] An analysis of arterial blood is used to determine the need for oxygen; this is recommended in those with an FEV1 less than 35% predicted, those with a peripheral oxygen saturation of less than 92% and those with symptoms of congestive heart failure.[9] In areas of the world where alpha-1 antitrypsin deficiency is common, people with COPD (particularly those below the age of 45 and with emphysema affecting the lower parts of the lungs) should be considered for testing.[9]
-
Chest X-ray demonstrating severe COPD. Note the small heart size in comparison to the lungs.
-
A lateral chest x-ray of a person with emphysema. Note the barrel chest and flat diaphragm.
-
Lung bulla as seen on CXR in a person with severe COPD
-
A severe case of bullous emphysema
-
Axial CT image of the lung of a person with end-stage bullous emphysema.
Ayırıcı tanı
COPD may need to be differentiated from other causes of shortness of breath such as congestive heart failure, pulmonary embolism, pneumonia or pneumothorax. Many people with COPD mistakenly think they have asthma.[16] The distinction between asthma and COPD is made on the basis of the symptoms, smoking history, and whether airflow limitation is reversible with bronchodilators at spirometry.[53] Tuberculosis may also present with a chronic cough and should be considered in locations where it is common.[9] Less common conditions that may present similarly include bronchopulmonary dysplasia and obliterative bronchiolitis.[51] Chronic bronchitis may occur with normal airflow and in this situation it is not classified as COPD.[2]
Önlem
Most cases of COPD are potentially preventable through decreasing exposure to smoke and improving air quality.[29] Annual influenza vaccinations in those with COPD reduce exacerbations, hospitalizations and death.[54][55] Pneumococcal vaccination may also be beneficial.[54]
Sigarayı bırakma
Keeping people from starting smoking is a key aspect of preventing COPD.[56] The policies of governments, public health agencies and anti-smoking organizations can reduce smoking rates by discouraging people from starting and encouraging people to stop smoking.[57] Smoking bans in public areas and places of work are important measures to decrease exposure to secondhand smoke and while many places have instituted bans more are recommended.[29]
In those who smoke, stopping smoking is the only measure shown to slow down the worsening of COPD.[58] Even at a late stage of the disease, it can reduce the rate of worsening lung function and delay the onset of disability and death.[59] Smoking cessation starts with the decision to stop smoking, leading to an attempt at quitting. Often several attempts are required before long-term abstinence is achieved.[57] Attempts over 5 years lead to success in nearly 40% of people.[60]
Some smokers can achieve long-term smoking cessation through willpower alone. Smoking, however, is highly addictive,[61] and many smokers need further support. The chance of quitting is improved with social support, engagement in a smoking cessation program and the use of medications such as nicotine replacement therapy, bupropion or varenicline.[57][60]
Meslek sağlığı
A number of measures have been taken to reduce the likelihood that workers in at-risk industries—such as coal mining, construction and stonemasonry—will develop COPD.[29] Examples of these measures include: the creation of public policy,[29] education of workers and management about the risks, promoting smoking cessation, checking workers for early signs of COPD, use of respirators, and dust control.[62][63] Effective dust control can be achieved by improving ventilation, using water sprays and by using mining techniques that minimize dust generation.[64] If a worker develops COPD, further lung damage can be reduced by avoiding ongoing dust exposure, for example by changing the work role.[65]
Hava kirliliği
Both indoor and outdoor air quality can be improved, which may prevent COPD or slow the worsening of existing disease.[29] This may be achieved by public policy efforts, cultural changes, and personal involvement.[66]
A number of developed countries have successfully improved outdoor air quality through regulations. This has resulted in improvements in the lung function of their populations.[29] Those with COPD may experience fewer symptoms if they stay indoors on days when outdoor air quality is poor.[4]
One key effort is to reduce exposure to smoke from cooking and heating fuels through improved ventilation of homes and better stoves and chimneys.[66] Proper stoves may improve indoor air quality by 85%. Using alternative energy sources such as solar cooking and electrical heating is effective, as is using fuels such as kerosene or coal rather than biomass.[29]
Yönetim
There is no known cure for COPD, but the symptoms are treatable and its progression can be delayed.[56] The major goals of management are to reduce risk factors, manage stable COPD, prevent and treat acute exacerbations, and manage associated illnesses.[4] The only measures that have been shown to reduce mortality are smoking cessation and supplemental oxygen.[67] Stopping smoking decreases the risk of death by 18%.[3] Other recommendations include influenza vaccination once a year, pneumococcal vaccination once every 5 years, and reduction in exposure to environmental air pollution.[3] In those with advanced disease, palliative care may reduce symptoms, with morphine improving the feelings of shortness of breath.[68] Noninvasive ventilation may be used to support breathing.[68]
Egzersiz
Pulmonary rehabilitation is a program of exercise, disease management and counseling, coordinated to benefit the individual.[69] In those who have had a recent exacerbation, pulmonary rehabilitation appears to improve the overall quality of life and the ability to exercise, and reduce mortality.[70] It has also been shown to improve the sense of control a person has over their disease, as well as their emotions.[71] Breathing exercises in and of themselves appear to have a limited role.[15]
Being either underweight or overweight can affect the symptoms, degree of disability and prognosis of COPD. People with COPD who are underweight can improve their breathing muscle strength by increasing their calorie intake.[4] When combined with regular exercise or a pulmonary rehabilitation program, this can lead to improvements in COPD symptoms. Supplemental nutrition may be useful in those who are malnourished.[72]
Bronkodilatörler
Inhaled bronchodilators are the primary medications used[3] and result in a small overall benefit.[73] There are two major types, β2 agonists and anticholinergics; both exist in long-acting and short-acting forms. They reduce shortness of breath, wheeze and exercise limitation, resulting in an improved quality of life.[74] It is unclear if they change the progression of the underlying disease.[3]
In those with mild disease, short-acting agents are recommended on an as needed basis.[3] In those with more severe disease, long-acting agents are recommended.[3] If long-acting bronchodilators are insufficient, then inhaled corticosteroids are typically added.[3] With respect to long-acting agents, it is unclear if tiotropium (a long-acting anticholinergic) or long-acting beta agonists (LABAs) are better, and it may be worth trying each and continuing the one that worked best.[75] Both types of agent appear to reduce the risk of acute exacerbations by 15–25%.[3] While both may be used at the same time, any benefit is of questionable significance.[76]
There are several short-acting β2 agonists available including salbutamol (Ventolin) and terbutaline.[77] They provide some relief of symptoms for four to six hours.[77] Long-acting β2 agonists such as salmeterol and formoterol are often used as maintenance therapy. Some feel the evidence of benefits is limited[78] while others view the evidence of benefit as established.[79][80] Long-term use appears safe in COPD[81] with adverse effects include shakiness and heart palpitations.[3] When used with inhaled steroids they increase the risk of pneumonia.[3] While steroids and LABAs may work better together,[78] it is unclear if this slight benefit outweighs the increased risks.[82]
There are two main anticholinergics used in COPD, ipratropium and tiotropium. Ipratropium is a short-acting agent while tiotropium is long-acting. Tiotropium is associated with a decrease in exacerbations and improved quality of life,[76] and tiotropium provides those benefits better than ipratropium.[83] It does not appear to affect mortality or the over all hospitalization rate.[84] Anticholinergics can cause dry mouth and urinary tract symptoms.[3] They are also associated with increased risk of heart disease and stroke.[85][86] Aclidinium, another long acting agent which came to market in 2012, has been used as an alternative to tiotropium.[87][88]
Kortikosteroitler
Corticosteroids are usually used in inhaled form but may also be used as tablets to treat and prevent acute exacerbations. While inhaled corticosteroids (ICS) have not shown benefit for people with mild COPD, they decrease acute exacerbations in those with either moderate or severe disease.[89] When used in combination with a LABA they decrease mortality more than either ICS or LABA alone.[90] By themselves they have no effect on overall one-year mortality and are associated with increased rates of pneumonia.[67] It is unclear if they affect the progression of the disease.[3] Long-term treatment with steroid tablets is associated with significant side effects.[77]
Diğer ilaçlar
Long-term antibiotics, specifically those from the macrolide class such as erythromycin, reduce the frequency of exacerbations in those who have two or more a year.[91][92] This practice may be cost effective in some areas of the world.[93] Concerns include that of antibiotic resistance and hearing problems with azithromycin.[92] Methylxanthines such as theophylline generally cause more harm than benefit and thus are usually not recommended,[94] but may be used as a second-line agent in those not controlled by other measures.[4] Mucolytics may be useful in some people who have very thick mucus but are generally not needed.[54] Cough medicines are not recommended.[77]
Oksijen
Supplemental oxygen is recommended in those with low oxygen levels at rest (a partial pressure of oxygen of less than 50–55 mmHg or oxygen saturations of less than 88%).[77][95] In this group of people it decreases the risk of heart failure and death if used 15 hours per day[77][95] and may improve people's ability to exercise.[96] In those with normal or mildly low oxygen levels, oxygen supplementation may improve shortness of breath.[97] There is a risk of fires and little benefit when those on oxygen continue to smoke.[98] In this situation some recommend against its use.[99] During acute exacerbations, many require oxygen therapy; the use of high concentrations of oxygen without taking into account a person's oxygen saturations may lead to increased levels of carbon dioxide and worsened outcomes.[100][101] In those at high risk of high carbon dioxide levels, oxygen saturations of 88–92% are recommended, while for those without this risk recommended levels are 94–98%.[101]
Cerrahi
For those with very severe disease surgery is sometimes helpful and may include lung transplantation or lung volume reduction surgery.[3] Lung volume reduction surgery involves removing the parts of the lung most damaged by emphysema allowing the remaining, relatively good lung to expand and work better.[77] Lung transplantation is sometimes performed for very severe COPD, particularly in younger individuals.[77]
Ataklar
Acute exacerbations are typically treated by increasing the usage of short-acting bronchodilators.[3] This commonly includes a combination of a short-acting inhaled beta agonist and anticholinergic.[37] These medications can be given either via a metered-dose inhaler with a spacer or via a nebulizer with both appearing to be equally effective.[37] Nebulization may be easier for those who are more unwell.[37]
Oral corticosteroids improve the chance of recovery and decrease the overall duration of symptoms.[3][37] They work equally well as intravenous steroids but appear to have fewer side effects.[102] Five days of steroids work as well as ten or fourteen.[103] In those with a severe exacerbation, antibiotics improve outcomes.[104] A number of different antibiotics may be used including amoxicillin, doxycycline and azithromycin; it is unclear if one is better than the others.[54] There is no clear evidence for those with less severe cases.[104]
For those with type 2 respiratory failure (acutely raised CO2 levels) non-invasive positive pressure ventilation decreases the probability of death or the need of intensive care admission.[3] Additionally, theophylline may have a role in those who do not respond to other measures.[3] Fewer than 20% of exacerbations require hospital admission.[37] In those without acidosis from respiratory failure, home care ("hospital at home") may be able to help avoid some admissions.[37][105]
Prognoz

no data ≤110 110–220 220–330 330–440 440–550 550–660 | 660–770 770–880 880–990 990–1100 1100–1350 ≥1350 |
COPD usually gets gradually worse over time and can ultimately result in death. It is estimated that 3% of all disability is related to COPD.[107] The proportion of disability from COPD globally has decreased from 1990 to 2010 due to improved indoor air quality primarily in Asia.[107] The overall number of years lived with disability from COPD, however, has increased.[108]
The rate at which COPD worsens varies with the presence of factors that predict a poor outcome, including severe airflow obstruction, little ability to exercise, shortness of breath, significantly underweight or overweight, congestive heart failure, continued smoking, and frequent exacerbations.[4] Long-term outcomes in COPD can be estimated using the BODE index which gives a score of zero to ten depending on FEV1, body-mass index, the distance walked in six minutes, and the modified MRC dyspnea scale.[109] Significant weight loss is a bad sign.[2] Results of spirometry are also a good predictor of the future progress of the disease but not as good as the BODE index.[2][10]
Epidemiyoloji
Globally, as of 2010, COPD affected approximately 329 million people (4.8% of the population) and is slightly more common in men than women.[108] This is as compared to 64 million being affected in 2004.[110] The increase in the developing world between 1970 and the 2000s is believed to be related to increasing rates of smoking in this region, an increasing population and an aging population due to less deaths from other causes such as infectious diseases.[3] Some developed countries have seen increased rates, some have remained stable and some have seen a decrease in COPD prevalence.[3] The global numbers are expected to continue increasing as risk factors remain common and the population continues to get older.[56]
Between 1990 and 2010 the number of deaths from COPD decreased slightly from 3.1 million to 2.9 million[111] and became the fourth leading cause of death.[3] In 2012 it became the third leading cause as the number of deaths rose again to 3.1 million.[6] In some countries, mortality has decreased in men but increased in women.[112] This is most likely due to rates of smoking in women and men becoming more similar.[2] COPD is more common in older people;[1] it affects 34-200 out of 1000 people older than 65 years, depending on the population under review.[1][52]
In England, an estimated 0.84 million people (of 50 million) have a diagnosis of COPD; this translates into approximately one person in 59 receiving a diagnosis of COPD at some point in their lives. In the most socioeconomically deprived parts of the country, one in 32 people were diagnosed with COPD, compared with one in 98 in the most affluent areas.[113] In the United States approximately 6.3% of the adult population, totaling approximately 15 million people, have been diagnosed with COPD.[114] 25 million people may have COPD if currently undiagnosed cases are included.[115] In 2011, there were approximately 730,000 hospitalizations in the United States for COPD.[116]
Tarih
The word "emphysema" is derived from the Greek Yunanca: ἐμφυσᾶν emphysan meaning "inflate" -itself composed of ἐν en, meaning "in", and φυσᾶν physan, meaning "breath, blastŞablon:-".[117] The term chronic bronchitis came into use in 1808[118] while the term COPD is believed to have first been used in 1965.[119] Previously it has been known by a number of different names, including chronic obstructive bronchopulmonary disease, chronic obstructive respiratory disease, chronic airflow obstruction, chronic airflow limitation, chronic obstructive lung disease, nonspecific chronic pulmonary disease, and diffuse obstructive pulmonary syndrome. The terms chronic bronchitis and emphysema were formally defined in 1959 at the CIBA guest symposium and in 1962 at the American Thoracic Society Committee meeting on Diagnostic Standards.[119]
Early descriptions of probable emphysema include: in 1679 by T. Bonet of a condition of "voluminous lungs" and in 1769 by Giovanni Morgagni of lungs which were "turgid particularly from air".[119][120] In 1721 the first drawings of emphysema were made by Ruysh.[120] These were followed with pictures by Matthew Baillie in 1789 and descriptions of the destructive nature of the condition. In 1814 Charles Badham used "catarrh" to describe the cough and excess mucus in chronic bronchitis. René Laennec, the physician who invented the stethoscope, used the term "emphysema" in his book A Treatise on the Diseases of the Chest and of Mediate Auscultation (1837) to describe lungs that did not collapse when he opened the chest during an autopsy. He noted that they did not collapse as usual because they were full of air and the airways were filled with mucus. In 1842, John Hutchinson invented the spirometer, which allowed the measurement of vital capacity of the lungs. However, his spirometer could only measure volume, not airflow. Tiffeneau and Pinelli in 1947 described the principles of measuring airflow.[119]
In 1953, Dr. George L. Waldbott, an American allergist, first described a new disease he named "smoker's respiratory syndrome" in the 1953 Journal of the American Medical Association. This was the first association between tobacco smoking and chronic respiratory disease.[121]
Early treatments included garlic, cinnamon and ipecac, among others.[118] Modern treatments were developed during the second half of the 20th century. Evidence supporting the use of steroids in COPD were published in the late 1950s. Bronchodilators came into use in the 1960s following a promising trial of isoprenaline. Further bronchodilators, such as salbutamol, were developed in the 1970s, and the use of LABAs began in the mid-1990s.[122]
Toplum ve kültür
COPD has been referred to as "smoker's lung".[123] Those with emphysema have been known as "pink puffers" or "type A" due to their frequent pink complexion, fast respiratory rate and pursed lips,[124][125] and people with chronic bronchitis have been referred to as "blue bloaters" or "type B" due to the often bluish color of the skin and lips from low oxygen levels and their ankle swelling.[125][126] This terminology is no longer accepted as useful as most people with COPD have a combination of both.[2][125]
Many health systems have difficulty ensuring appropriate identification, diagnosis and care of people with COPD; Britain's Department of Health has identified this as a major issue for the National Health Service and has introduced a specific strategy to tackle these problems.[127]
Ekonomi
Globally, as of 2010, COPD is estimated to result in economic costs of $2.1 trillion, half of which occurring in the developing world.[8] Of this total an estimated $1.9 trillion are direct costs such as medical care, while $0.2 trillion are indirect costs such as missed work.[128] This is expected to more than double by the year 2030.[8] In Europe, COPD represents 3% of healthcare spending.[1] In the United States, costs of the disease are estimated at $50 billion, most of which is due to exacerbation.[1] COPD was among the most expensive conditions seen in U.S. hospitals in 2011, with a total cost of about $5.7 billion.[116]
Araştırma
Infliximab, an immune-suppressing antibody, has been tested in COPD but there was no evidence of benefit with the possibility of harm.[129] Roflumilast shows promise in decreasing the rate of exacerbations but does not appear to change quality of life.[3] A number of new, long-acting agents are under development.[3] Treatment with stem cells is under study,[130] and while generally safe and with promising animal data there is little human data as of 2014.[131]
Diğer hayvanlar
Chronic obstructive pulmonary disease may occur in a number of other animals and may be caused by exposure to tobacco smoke.[132][133] Most cases of the disease, however, are relatively mild.[134] In horses it is also known as recurrent airway obstruction and is typically due to an allergic reaction to a fungus contained in straw.[135] COPD is also commonly found in old dogs.[136]
Ayrıca bakınız
Bibliyografi
- "Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease, Updated 2013" (PDF). Global Initiative for Chronic Obstructive Lung Disease. Erişim tarihi: November 29, 2013.
- Şablon:NICE
- Qaseem, Amir; Wilt, TJ; Weinberger, SE; Hanania, NA; Criner, G; Van Der Molen, T; Marciniuk, DD; Denberg, T; Schünemann, H; Wedzicha, W; MacDonald, R; Shekelle, P; American College Of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society (2011). "Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease: A Clinical Practice Guideline Update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society". Annals of Internal Medicine. 155 (3): 179–91. doi:10.7326/0003-4819-155-3-201108020-00008. PMID 21810710.
Dış bağlantılar
| Wikimedia Commons'ta Kronik obstrüktif akciğer hastalığı ile ilgili ortam dosyaları bulunmaktadır. |
- Curlie'de Kronik obstrüktif akciğer hastalığı (DMOZ tabanlı)
- Türk Toraks Derneği
| Wikimedia Commons'ta Kronik obstrüktif akciğer hastalığı ile ilgili ortam dosyaları bulunmaktadır. |
Kaynakça
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa Vestbo, Jørgen (2013). "Definition and Overview" (PDF). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease. ss. 1–7.
- ^ a b c d e f g h i j k l m n Reilly, John J.; Silverman, Edwin K.; Shapiro, Steven D. (2011). "Chronic Obstructive Pulmonary Disease". Longo, Dan; Fauci, Anthony; Kasper, Dennis; Hauser, Stephen; Jameson, J.; Loscalzo, Joseph (Ed.). Harrison's Principles of Internal Medicine (18th bas.). McGraw Hill. ss. 2151–9. ISBN 978-0-07-174889-6.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab Decramer M, Janssens W, Miravitlles M (Nisan 2012). "Chronic obstructive pulmonary disease". Lancet. 379 (9823): 1341–51. doi:10.1016/S0140-6736(11)60968-9. PMID 22314182.
- ^ a b c d e f g h i j k Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J (Eylül 2007). "Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary". Am. J. Respir. Crit. Care Med. 176 (6): 532–55. doi:10.1164/rccm.200703-456SO. PMID 17507545.
- ^ Nathell L, Nathell M, Malmberg P, Larsson K (2007). "COPD diagnosis related to different guidelines and spirometry techniques". Respir. Res. 8 (1): 89. doi:10.1186/1465-9921-8-89. PMC 2217523 $2. PMID 18053200.
- ^ a b "The 10 leading causes of death in the world, 2000 and 2011". World Health Organization. July 2013. Erişim tarihi: 29 Kasım 2013.
- ^ Mathers CD, Loncar D (November 2006). "Projections of Global Mortality and Burden of Disease from 2002 to 2030". PLoS Med. 3 (11): e442. doi:10.1371/journal.pmed.0030442. PMC 1664601 $2. PMID 17132052.
- ^ a b c Lomborg, Bjørn (2013). Global problems, local solutions : costs and benefits. Cambridge University Pres. s. 143. ISBN 978-1-107-03959-9.
- ^ a b c d e f g h i j k l m n o p q r s t u Vestbo, Jørgen (2013). "Diagnosis and Assessment" (PDF). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease. ss. 9–17.
- ^ a b c d e f g Şablon:NICE
- ^ Mahler DA (2006). "Mechanisms and measurement of dyspnea in chronic obstructive pulmonary disease". Proceedings of the American Thoracic Society. 3 (3): 234–8. doi:10.1513/pats.200509-103SF. PMID 16636091.
- ^ "What Are the Signs and Symptoms of COPD?". National Heart, Lung, and Blood Institute. 31 Temmuz 2013. Erişim tarihi: 29 Kasım 2013.
- ^ MedlinePlus Encyclopedia Chronic obstructive pulmonary disease
- ^ Morrison, [edited by] Nathan E. Goldstein, R. Sean (2013). Evidence-based practice of palliative medicine. Philadelphia: Elsevier/Saunders. s. 124. ISBN 978-1-4377-3796-7.
- ^ a b Holland AE, Hill CJ, Jones AY, McDonald CF (2012). Holland, Anne E (Ed.). "Breathing exercises for chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 10: CD008250. doi:10.1002/14651858.CD008250.pub2. PMID 23076942.
- ^ a b c d e f Gruber, Phillip (Kasım 2008). "The Acute Presentation of Chronic Obstructive Pulmonary Disease In the Emergency Department: A Challenging Oxymoron". Emergency Medicine Practice. 10 (11).
- ^ a b Weitzenblum E, Chaouat A (2009). "Cor pulmonale". Chron Respir Dis. 6 (3): 177–85. doi:10.1177/1479972309104664. PMID 19643833.
- ^ "Cor pulmonale". Professional guide to diseases (9th bas.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2009. ss. 120–2. ISBN 978-0-7817-7899-2.
- ^ Mandell, editors, James K. Stoller, Franklin A. Michota, Jr., Brian F. (2009). The Cleveland Clinic Foundation intensive review of internal medicine (5th bas.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. s. 419. ISBN 978-0-7817-9079-6.
- ^ Brulotte CA, Lang ES (May 2012). "Acute exacerbations of chronic obstructive pulmonary disease in the emergency department". Emerg. Med. Clin. North Am. 30 (2): 223–47, vii. doi:10.1016/j.emc.2011.10.005. PMID 22487106.
- ^ Spiro, Stephen (2012). Clinical respiratory medicine expert consult (4th bas.). Philadelphia, PA: Saunders. ISBN 978-1-4557-2329-4.
- ^ World Health Organization (2008). WHO Report on the Global Tobacco Epidemic 2008: The MPOWER Package (PDF). Geneva: World Health Organization. ss. 268–309. ISBN 92-4-159628-7.
- ^ a b Ward, Helen (2012). Oxford Handbook of Epidemiology for Clinicians. Oxford University Press. ss. 289–290. ISBN 978-0-19-165478-7.
- ^ Laniado-Laborín, R (January 2009). "Smoking and chronic obstructive pulmonary disease (COPD). Parallel epidemics of the 21st century". International journal of environmental research and public health. 6 (1): 209–24. doi:10.3390/ijerph6010209. PMC 2672326 $2. PMID 19440278.
- ^ a b Rennard, Stephen (2013). Clinical management of chronic obstructive pulmonary disease (2nd bas.). New York: Informa Healthcare. s. 23. ISBN 978-0-8493-7588-0.
- ^ a b Anita Sharma ; with a contribution by David Pitchforth ; forewords by Gail Richards; Barclay, Joyce (2010). COPD in primary care. Oxford: Radcliffe Pub. s. 9. ISBN 978-1-84619-316-3.
- ^ Goldman, Lee (2012). Goldman's Cecil medicine (24th bas.). Philadelphia: Elsevier/Saunders. s. 537. ISBN 978-1-4377-1604-7.
- ^ a b Kennedy SM, Chambers R, Du W, Dimich-Ward H (December 2007). "Environmental and occupational exposures: do they affect chronic obstructive pulmonary disease differently in women and men?". Proceedings of the American Thoracic Society. 4 (8): 692–4. doi:10.1513/pats.200707-094SD. PMID 18073405.
- ^ a b c d e f g h i j k l m Pirozzi C, Scholand MB (July 2012). "Smoking cessation and environmental hygiene". Med. Clin. North Am. 96 (4): 849–67. doi:10.1016/j.mcna.2012.04.014. PMID 22793948.
- ^ Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM (September 2006). "Global burden of COPD: systematic review and meta-analysis". Eur. Respir. J. 28 (3): 523–32. doi:10.1183/09031936.06.00124605. PMID 16611654.
- ^ a b Devereux, Graham (2006). "Definition, epidemiology and risk factors". BMJ. 332 (7550): 1142–4. doi:10.1136/bmj.332.7550.1142. PMC 1459603 $2. PMID 16690673.
- ^ Laine, Christine (2009). In the Clinic: Practical Information about Common Health Problems. ACP Press. s. 226. ISBN 978-1-934465-64-6.
- ^ a b Barnes, Peter J.; Drazen, Jeffrey M.; Rennard, Stephen I.; Thomson, Neil C., (Ed.) (2009). "Relationship between cigarette smoking and occupational exposures". Asthma and COPD: Basic Mechanisms and Clinical Management. Amsterdam: Academic. s. 464. ISBN 978-0-12-374001-4. Bilinmeyen parametre
|displayeditors=görmezden gelindi (yardım) - ^ Rushton, Lesley (2007). "Chronic Obstructive Pulmonary Disease and Occupational Exposure to Silica". Reviews on Environmental Health. 22 (4): 255–72. doi:10.1515/REVEH.2007.22.4.255. PMID 18351226.
- ^ a b c d Foreman MG, Campos M, Celedón JC (July 2012). "Genes and chronic obstructive pulmonary disease". Med. Clin. North Am. 96 (4): 699–711. doi:10.1016/j.mcna.2012.02.006. PMC 3399759 $2. PMID 22793939.
- ^ Brode SK, Ling SC, Chapman KR (September 2012). "Alpha-1 antitrypsin deficiency: a commonly overlooked cause of lung disease". CMAJ. 184 (12): 1365–71. doi:10.1503/cmaj.111749. PMC 3447047 $2. PMID 22761482.
- ^ a b c d e f g Vestbo, Jørgen (2013). "Management of Exacerbations" (PDF). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease. ss. 39–45.
- ^ a b c Dhar, Raja (2011). Textbook of pulmonary and critical care medicine. New Delhi: Jaypee Brothers Medical Publishers. s. 1056. ISBN 978-93-5025-073-0.
- ^ Palange, Paolo (2013). ERS Handbook of Respiratory Medicine. European Respiratory Society. s. 194. ISBN 978-1-84984-041-5.
- ^ Lötvall, Jan (2011). Advances in combination therapy for asthma and COPD. Chichester, West Sussex: John Wiley & Sons. s. 251. ISBN 978-1-119-97846-6.
- ^ Barnes, Peter (2009). Asthma and COPD : basic mechanisms and clinical management (2nd bas.). Amsterdam: Academic. s. 837. ISBN 978-0-12-374001-4.
- ^ Hanania, Nicola (2010-12-09). COPD a Guide to Diagnosis and Clinical Management (1st bas.). Totowa, NJ: Springer Science+Business Media, LLC. s. 197. ISBN 978-1-59745-357-8.
- ^ a b Beasley, V; Joshi, PV; Singanayagam, A; Molyneaux, PL; Johnston, SL; Mallia, P (2012). "Lung microbiology and exacerbations in COPD". International journal of chronic obstructive pulmonary disease. 7: 555–69. doi:10.2147/COPD.S28286. PMC 3437812 $2. PMID 22969296.
- ^ Murphy DMF, Fishman AP (2008). "Chapter 53". Fishman's Pulmonary Diseases and Disorders (4th bas.). McGraw-Hill. s. 913. ISBN 0-07-145739-9.
- ^ a b Calverley PM, Koulouris NG (2005). "Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology". Eur Respir J. 25 (1): 186–199. doi:10.1183/09031936.04.00113204. PMID 15640341.
- ^ Currie, Graeme P. (2010). ABC of COPD (2nd bas.). Chichester, West Sussex, UK: Wiley-Blackwell, BMJ Books. s. 32. ISBN 978-1-4443-2948-3.
- ^ O'Donnell DE (2006). "Hyperinflation, Dyspnea, and Exercise Intolerance in Chronic Obstructive Pulmonary Disease". The Proceedings of the American Thoracic Society. 3 (2): 180–4. doi:10.1513/pats.200508-093DO. PMID 16565429.
- ^ a b c d e f Qaseem, Amir; Wilt, TJ; Weinberger, SE; Hanania, NA; Criner, G; Van Der Molen, T; Marciniuk, DD; Denberg, T; Schünemann, H; Wedzicha, W; MacDonald, R; Shekelle, P; American College Of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society (2011). "Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease: A Clinical Practice Guideline Update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society". Annals of Internal Medicine. 155 (3): 179–91. doi:10.7326/0003-4819-155-3-201108020-00008. PMID 21810710.
- ^ a b Young, Vincent B. (2010). Blueprints medicine (5th bas.). Philadelphia: Wolters Kluwer Health/Lippincott William & Wilkins. s. 69. ISBN 978-0-7817-8870-0.
- ^ "COPD Assessment Test (CAT)". American Thoracic Society. Erişim tarihi: November 29, 2013.
- ^ a b Şablon:NICE
- ^ a b Torres M, Moayedi S (May 2007). "Evaluation of the acutely dyspneic elderly patient". Clin. Geriatr. Med. 23 (2): 307–25, vi. doi:10.1016/j.cger.2007.01.007. PMID 17462519.
- ^ BTS COPD Consortium (2005). "Spirometry in practice - a practical guide to using spirometry in primary care". ss. 8–9. Erişim tarihi: 25 August 2014.
- ^ a b c d Mackay AJ, Hurst JR (July 2012). "COPD exacerbations: causes, prevention, and treatment". Med. Clin. North Am. 96 (4): 789–809. doi:10.1016/j.mcna.2012.02.008. PMID 22793945.
- ^ Poole PJ, Chacko E, Wood-Baker RW, Cates CJ (2006). Poole, Phillippa (Ed.). "Influenza vaccine for patients with chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 1: CD002733. doi:10.1002/14651858.CD002733.pub2. PMID 16437444.
- ^ a b c Vestbo, Jørgen (2013). "Introduction". Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (PDF). Global Initiative for Chronic Obstructive Lung Disease. xiii–xv.
- ^ a b c Policy Recommendations for Smoking Cessation and Treatment of Tobacco Dependence. World Health Organization. ss. 15–40. ISBN 978-92-4-156240-9.
- ^ Jiménez-Ruiz CA, Fagerström KO (March 2013). "Smoking cessation treatment for COPD smokers: the role of counselling". Monaldi Arch Chest Dis. 79 (1): 33–7. PMID 23741944.
- ^ Kumar P, Clark M (2005). Clinical Medicine (6th bas.). Elsevier Saunders. ss. 900–1. ISBN 0-7020-2763-4.
- ^ a b Tønnesen P (March 2013). "Smoking cessation and COPD". Eur Respir Rev. 22 (127): 37–43. doi:10.1183/09059180.00007212. PMID 23457163.
- ^ "Why is smoking addictive?". NHS Choices. December 29, 2011. Erişim tarihi: November 29, 2013.
- ^ Smith, Barbara K. Timby, Nancy E. (2005). Essentials of nursing : care of adults and children. Philadelphia: Lippincott Williams & Wilkins. s. 338. ISBN 978-0-7817-5098-1.
- ^ Rom, William N.; Markowitz, Steven B., (Ed.) (2007). Environmental and occupational medicine (4th bas.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. ss. 521–2. ISBN 978-0-7817-6299-1.
- ^ "Wet cutting". Health and Safety Executive. Erişim tarihi: November 29, 2013.
- ^ George, Ronald B. (2005). Chest medicine : essentials of pulmonary and critical care medicine (5th bas.). Philadelphia, PA: Lippincott Williams & Wilkins. s. 172. ISBN 978-0-7817-5273-2.
- ^ a b Vestbo, Jørgen (2013). "Management of Stable COPD". Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (PDF). Global Initiative for Chronic Obstructive Lung Disease. ss. 31–8.
- ^ a b Drummond MB, Dasenbrook EC, Pitz MW, Murphy DJ, Fan E (November 2008). "Inhaled corticosteroids in patients with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis". JAMA. 300 (20): 2407–16. doi:10.1001/jama.2008.717. PMID 19033591.
- ^ a b Carlucci A, Guerrieri A, Nava S (December 2012). "Palliative care in COPD patients: is it only an end-of-life issue?". Eur Respir Rev. 21 (126): 347–54. doi:10.1183/09059180.00001512. PMID 23204123.
- ^ "COPD — Treatment". U.S. National Heart Lung and Blood Institute. Erişim tarihi: 2013-07-23.
- ^ Puhan MA, Gimeno-Santos E, Scharplatz M, Troosters T, Walters EH, Steurer J (2011). Puhan, Milo A (Ed.). "Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev (10): CD005305. doi:10.1002/14651858.CD005305.pub3. PMID 21975749.
- ^ Lacasse Y, Goldstein R, Lasserson TJ, Martin S (2006). Lacasse, Yves (Ed.). "Pulmonary rehabilitation for chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 4: CD003793. doi:10.1002/14651858.CD003793.pub2. PMID 17054186.
- ^ Ferreira IM, Brooks D, White J, Goldstein R (2012). Ferreira, Ivone M (Ed.). "Nutritional supplementation for stable chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 12: CD000998. doi:10.1002/14651858.CD000998.pub3. PMID 23235577.
- ^ van Dijk WD, van den Bemt L, van Weel C (2013). "Megatrials for bronchodilators in chronic obstructive pulmonary disease (COPD) treatment: time to reflect". J Am Board Fam Med. 26 (2): 221–4. doi:10.3122/jabfm.2013.02.110342. PMID 23471939.
- ^ Liesker JJ, Wijkstra PJ, Ten Hacken NH, Koëter GH, Postma DS, Kerstjens HA (February 2002). "A systematic review of the effects of bronchodilators on exercise capacity in patients with COPD". Chest. 121 (2): 597–608. doi:10.1378/chest.121.2.597. PMID 11834677.
- ^ Chong J, Karner C, Poole P (2012). Chong, Jimmy (Ed.). "Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 9: CD009157. doi:10.1002/14651858.CD009157.pub2. PMID 22972134.
- ^ a b Karner C, Cates CJ (2012). Karner, Charlotta (Ed.). "Long-acting beta(2)-agonist in addition to tiotropium versus either tiotropium or long-acting beta(2)-agonist alone for chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 4: CD008989. doi:10.1002/14651858.CD008989.pub2. PMID 22513969. Kaynak hatası: Geçersiz
<ref>etiketi: "Karner2012" adı farklı içerikte birden fazla tanımlanmış (Bkz: Kaynak gösterme) - ^ a b c d e f g h Vestbo, Jørgen (2013). "Therapeutic Options" (PDF). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease. ss. 19–30.
- ^ a b Cave, AC.; Hurst, MM. (May 2011). "The use of long acting β₂-agonists, alone or in combination with inhaled corticosteroids, in chronic obstructive pulmonary disease (COPD): a risk-benefit analysis". Pharmacol Ther. 130 (2): 114–43. doi:10.1016/j.pharmthera.2010.12.008. PMID 21276815.
- ^ Spencer, S; Karner, C; Cates, CJ; Evans, DJ (Dec 7, 2011). Spencer, Sally (Ed.). "Inhaled corticosteroids versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease". Cochrane Database Syst Rev (12): CD007033. doi:10.1002/14651858.CD007033.pub3. PMID 22161409.
- ^ Wang, J; Nie, B; Xiong, W; Xu, Y (April 2012). "Effect of long-acting beta-agonists on the frequency of COPD exacerbations: a meta-analysis". Journal of clinical pharmacy and therapeutics. 37 (2): 204–11. doi:10.1111/j.1365-2710.2011.01285.x. PMID 21740451.
- ^ Decramer ML, Hanania NA, Lötvall JO, Yawn BP (2013). "The safety of long-acting β2-agonists in the treatment of stable chronic obstructive pulmonary disease". Int J Chron Obstruct Pulmon Dis. 8: 53–64. doi:10.2147/COPD.S39018. PMC 3558319 $2. PMID 23378756.
- ^ Nannini, LJ; Lasserson, TJ; Poole, P (Sep 12, 2012). Nannini, Luis Javier (Ed.). "Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 9: CD006829. doi:10.1002/14651858.CD006829.pub2. PMID 22972099.
- ^ Cheyne L, Irvin-Sellers MJ, White J (Sep 16, 2013). Cheyne, Leanne (Ed.). "Tiotropium versus ipratropium bromide for chronic obstructive pulmonary disease". Cochrane Database of Systematic Reviews. 9 (9): CD009552. doi:10.1002/14651858.CD009552.pub2. PMID 24043433.
- ^ Karner, C; Chong, J; Poole, P (Jul 11, 2012). Karner, Charlotta (Ed.). "Tiotropium versus placebo for chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 7: CD009285. doi:10.1002/14651858.CD009285.pub2. PMID 22786525.
- ^ Singh S, Loke YK, Furberg CD (September 2008). "Inhaled anticholinergics and risk of major adverse cardiovascular events in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis". JAMA. 300 (12): 1439–50. doi:10.1001/jama.300.12.1439. PMID 18812535.
- ^ Singh S, Loke YK, Enright P, Furberg CD (January 2013). "Pro-arrhythmic and pro-ischaemic effects of inhaled anticholinergic medications". Thorax. 68 (1): 114–6. doi:10.1136/thoraxjnl-2011-201275. PMID 22764216.
- ^ Jones, P (Apr 2013). "Aclidinium bromide twice daily for the treatment of chronic obstructive pulmonary disease: a review". Advances in therapy. 30 (4): 354–68. doi:10.1007/s12325-013-0019-2. PMID 23553509.
- ^ Cazzola, M; Page, CP; Matera, MG (Jun 2013). "Aclidinium bromide for the treatment of chronic obstructive pulmonary disease". Expert opinion on pharmacotherapy. 14 (9): 1205–14. doi:10.1517/14656566.2013.789021. PMID 23566013.
- ^ Gartlehner G, Hansen RA, Carson SS, Lohr KN (2006). "Efficacy and Safety of Inhaled Corticosteroids in Patients With COPD: A Systematic Review and Meta-Analysis of Health Outcomes". Ann Fam Med. 4 (3): 253–62. doi:10.1370/afm.517. PMC 1479432 $2. PMID 16735528.
- ^ Shafazand S (June 2013). "ACP Journal Club. Review: inhaled medications vary substantively in their effects on mortality in COPD". Ann. Intern. Med. 158 (12): JC2. doi:10.7326/0003-4819-158-12-201306180-02002. PMID 23778926.
- ^ Mammen MJ, Sethi S (2012). "Macrolide therapy for the prevention of acute exacerbations in chronic obstructive pulmonary disease". Pol. Arch. Med. Wewn. 122 (1–2): 54–9. PMID 22353707.
- ^ a b Herath, SC; Poole, P (Nov 28, 2013). "Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD)". Cochrane Database Syst Rev. 11: CD009764. doi:10.1002/14651858.CD009764.pub2. PMID 24288145.
- ^ Simoens, S; Laekeman, G; Decramer, M (May 2013). "Preventing COPD exacerbations with macrolides: a review and budget impact analysis". Respiratory medicine. 107 (5): 637–48. doi:10.1016/j.rmed.2012.12.019. PMID 23352223.
- ^ Barr RG, Rowe BH, Camargo CA (2003). Barr, R Graham (Ed.). "Methylxanthines for exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev (2): CD002168. doi:10.1002/14651858.CD002168. PMID 12804425.
- ^ a b COPD Working, Group (2012). "Long-term oxygen therapy for patients with chronic obstructive pulmonary disease (COPD): an evidence-based analysis". Ontario health technology assessment series. 12 (7): 1–64. PMC 3384376 $2. PMID 23074435.
- ^ Bradley JM, O'Neill B (2005). Bradley, Judy M (Ed.). "Short-term ambulatory oxygen for chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 4: CD004356. doi:10.1002/14651858.CD004356.pub3. PMID 16235359.
- ^ Uronis H, McCrory DC, Samsa G, Currow D, Abernethy A (2011). Abernethy, Amy (Ed.). "Symptomatic oxygen for non-hypoxaemic chronic obstructive pulmonary disease". Cochrane Database Syst Rev (6): CD006429. doi:10.1002/14651858.CD006429.pub2. PMID 21678356.
- ^ Chapman, Stephen (2009). Oxford handbook of respiratory medicine (2nd bas.). Oxford: Oxford University Press. s. 707. ISBN 978-0-19-954516-2.
- ^ Blackler, Laura (2007). Managing chronic obstructive pulmonary disease. Chichester, England: John Wiley & Sons. s. 49. ISBN 978-0-470-51798-7.
- ^ Jindal, Surinder K (2013). Chronic Obstructive Pulmonary Disease. Jaypee Brothers Medical. s. 139. ISBN 978-93-5090-353-7.
- ^ a b O'Driscoll, BR; Howard, LS; Davison, AG; British Thoracic, Society (October 2008). "BTS guideline for emergency oxygen use in adult patients". Thorax. 63 (Suppl 6): vi1–68. doi:10.1136/thx.2008.102947. PMID 18838559.
- ^ Walters, JA; Tan, DJ; White, CJ; Gibson, PG; Wood-Baker, R; Walters, EH (September 2014). "Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 9: CD001288. doi:10.1002/14651858.CD001288.pub4. PMID 25178099.
- ^ Walters, JA; Tan, DJ; White, CJ; Wood-Baker, R (10 December 2014). "Different durations of corticosteroid therapy for exacerbations of chronic obstructive pulmonary disease". The Cochrane database of systematic reviews. 12: CD006897. PMID 25491891.
- ^ a b Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA (2012). Vollenweider, Daniela J (Ed.). "Antibiotics for exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 12: CD010257. doi:10.1002/14651858.CD010257. PMID 23235687.
- ^ Jeppesen, E; Brurberg, KG; Vist, GE; Wedzicha, JA; Wright, JJ; Greenstone, M; Walters, JA (May 16, 2012). "Hospital at home for acute exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 5: CD003573. doi:10.1002/14651858.CD003573.pub2. PMID 22592692.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Erişim tarihi: Nov 11, 2009.
- ^ a b Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA; ve diğerleri. (December 2012). "Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2197–223. doi:10.1016/S0140-6736(12)61689-4. PMID 23245608.
- ^ a b Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V; ve diğerleri. (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ^ Medicine, prepared by the Department of Medicine, Washington University School of (2009). The Washington manual general internal medicine subspecialty consult (2nd bas.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. s. 96. ISBN 978-0-7817-9155-7.
- ^ "Chronic obstructive pulmonary disease (COPD) Fact sheet N°315". WHO. November 2012.
- ^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R; ve diğerleri. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
- ^ Rycroft CE, Heyes A, Lanza L, Becker K (2012). "Epidemiology of chronic obstructive pulmonary disease: a literature review". Int J Chron Obstruct Pulmon Dis. 7: 457–94. doi:10.2147/COPD.S32330. PMC 3422122 $2. PMID 22927753.
- ^ Simpson CR, Hippisley-Cox J, Sheikh A (2010). "Trends in the epidemiology of chronic obstructive pulmonary disease in England: a national study of 51 804 patients". Brit J Gen Pract. 60 (576): 483–8. doi:10.3399/bjgp10X514729. PMC 2894402 $2. PMID 20594429.
- ^ Centers for Disease Control and Prevention (Nov 23, 2012). "Chronic Obstructive Pulmonary Disease Among Adults — United States, 2011". Morbidity and Mortality Weekly Report. 61 (46): 938–43. PMID 23169314.
- ^ "Morbidity & Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases" (PDF). National Heart, Lung, and Blood Institute.
- ^ a b Torio CM, Andrews RM (2006). "National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011: Statistical Brief #160". Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Health Care Policy and Research. PMID 24199255.
- ^ "Emphysema". Dictionary.com. Erişim tarihi: 21 November 2013.
- ^ a b Ziment, Irwin (1991). "History of the Treatment of Chronic Bronchitis". Respiration. 58 (Suppl 1): 37–42. doi:10.1159/000195969. PMID 1925077.
- ^ a b c d Petty TL (2006). "The history of COPD". Int J Chron Obstruct Pulmon Dis. 1 (1): 3–14. doi:10.2147/copd.2006.1.1.3. PMC 2706597 $2. PMID 18046898.
- ^ a b Wright, Joanne L.; Churg, Andrew (2008). "Pathologic Features of Chronic Obstructive Pulmonary Disease: Diagnostic Criteria and Differential Diagnosis" (PDF). Fishman, Alfred; Elias, Jack; Fishman, Jay; Grippi, Michael; Senior, Robert; Pack, Allan (Ed.). Fishman's Pulmonary Diseases and Disorders (4th bas.). New York: McGraw-Hill. ss. 693–705. ISBN 978-0-07-164109-8.
- ^ George L. Waldbott (1965). A struggle with Titans. Carlton Press. s. 6.
- ^ Fishman AP (May 2005). "One hundred years of chronic obstructive pulmonary disease". Am. J. Respir. Crit. Care Med. 171 (9): 941–8. doi:10.1164/rccm.200412-1685OE. PMID 15849329.
- ^ Yuh-Chin, T. Huang (2012-10-28). A clinical guide to occupational and environmental lung diseases. [New York]: Humana Press. s. 266. ISBN 978-1-62703-149-3.
- ^ "Pink Puffer - definition of Pink Puffer in the Medical dictionary - by the Free Online Medical Dictionary, Thesaurus and Encyclopedia". Medical-dictionary.thefreedictionary.com. Erişim tarihi: 2013-07-23.
- ^ a b c Weinberger, Steven E. (2013-05-08). Principles of pulmonary medicine (6th bas.). Philadelphia: Elsevier/Saunders. s. 165. ISBN 978-1-62703-149-3.
- ^ Des Jardins, Terry (2013). Clinical Manifestations & Assessment of Respiratory Disease (6th bas.). Elsevier Health Sciences. s. 176. ISBN 978-0-323-27749-5.
- ^ An outcomes strategy for people with chronic obstructive pulmonary disease (COPD) and asthma in England (PDF). Department of Health. 18 July 2011. s. 5. Erişim tarihi: 27 November 2013.
- ^ Bloom, D (2011). The Global Economic Burden of Noncommunicable Diseases (PDF). World Economic Forum. s. 24.
- ^ Nici, Linda (2011). Chronic Obstructive Pulmonary Disease: Co-Morbidities and Systemic Consequences. Springer. s. 78. ISBN 978-1-60761-673-3.
- ^ Inamdar, AC; Inamdar, AA (Oct 2013). "Mesenchymal stem cell therapy in lung disorders: pathogenesis of lung diseases and mechanism of action of mesenchymal stem cell". Experimental lung research. 39 (8): 315–27. doi:10.3109/01902148.2013.816803. PMID 23992090.
- ^ Conese, M; Piro, D; Carbone, A; Castellani, S; Di Gioia, S (2014). "Hematopoietic and mesenchymal stem cells for the treatment of chronic respiratory diseases: role of plasticity and heterogeneity". TheScientificWorldJournal. 2014: 859817. doi:10.1155/2014/859817. PMC 3916026 $2. PMID 24563632.
- ^ Akers, R. Michael; Denbow, D. Michael (2008). Anatomy and Physiology of Domestic Animals. Arnes, AI: Wiley. s. 852. ISBN 978-1-118-70115-7.
- ^ Wright, JL; Churg, A (December 2002). "Animal models of cigarette smoke-induced COPD". Chest. 122 (6 Suppl): 301S–6S. doi:10.1378/chest.122.6_suppl.301S. PMID 12475805.
- ^ Churg, A; Wright, JL (2007). "Animal models of cigarette smoke-induced chronic obstructive lung disease". Contributions to microbiology. Contributions to Microbiology. 14: 113–25. doi:10.1159/000107058. ISBN 3-8055-8332-X. PMID 17684336.
- ^ Marinkovic D, Aleksic-Kovacevic S, Plamenac P (2007). "Cellular basis of chronic obstructive pulmonary disease in horses". Int. Rev. Cytol. International Review of Cytology. 257: 213–47. doi:10.1016/S0074-7696(07)57006-3. ISBN 978-0-12-373701-4. PMID 17280899.
- ^ Miller MS, Tilley LP, Smith FW (January 1989). "Cardiopulmonary disease in the geriatric dog and cat". Vet. Clin. North Am. Small Anim. Pract. 19 (1): 87–102. PMID 2646821.







